Diagnostic Laparoscopy
Diagnostic laparoscopy is a minimally invasive surgical procedure that allows the visual examination of intraabdominal organs in order to detect pathology. The procedure allows the direct visual examination of intraabdominal organs including large surface areas of the liver, gallbladder, spleen, peritoneum, pelvic organs, and retroperitoneum. Biopsies, aspiration, and cultures can be obtained, and laparoscopic ultrasound may be used.
Diagnostic laparoscopy is safe and well-tolerated and can be performed in an outpatient or inpatient setting under general anesthesia. There may also be unique circumstances where office-based diagnostic laparoscopy may be considered under local anesthesia. These circumstances should include only procedures where complications and the need for therapeutic procedures through the same access are extremely unlikely. Manipulation and biopsy of the viscera are possible through additional ports. Diagnostic laparoscopy is the most commonly performed gynecological procedure today. Its greatest advantage is that it has replaced exploratory laparotomy.
Diagnostic laparoscopy was first introduced in 1901, when Kelling, performed a peritoneoscopy in a dog and was called ‘‘celioscopy’’. A Swedish internist named Jacobaeusc is credited with performing the first diagnostic laparoscopy on humans in 1910. He described its application in patients with ascites and for the early diagnosis of malignant lesions. In the last ten years, laparoscopy has made a great difference to the diagnosis of abdominal acute and chronic pain. It has evolved as an informative important method of diagnosing a wide spectrum of both benign and malignant diseases. Elective diagnostic laparoscopy refers to the use of the procedure in chronic intra-abdominal disorders. Emergency diagnostic laparoscopy is performed in patients presenting with an acute abdomen.
Indications
The indications for diagnostic laparoscopy can be divided into two main groups.
Non-traumatic, Non-gynecological Acute Abdomen Like:
• Appendicitis
• Diverticulitis
• Duodenal perforation
• Mesenteric adenitis
• Intestinal adhesion
• Omental necrosis
• Intestinal infarction
• Complicated Meckel’s diverticulum
• Bedside laparoscopy in the ICU
• Torsion of the intra-abdominal testis.
Gynecological Abdominal Emergencies Like:
• Ovarian cysts
• Pelvic inflammatory diseases
• Acute salpingitis
• Ectopic pregnancy
• Endometriosis
• Perforated uterus due to criminal abortion
• Salpingitis.
One of the important uses for diagnostic laparoscopy is the investigation of female infertility. Tubal causes of infertility are found in 15 percent of a couple. In these patients, laparoscopy not only allows tubal patency to be assessed but also enables other features in the pelvis to be examined. The most important findings related to infertility are kinking of the tube, fimbrial damage, or ovarian adhesions. The presence of corpus luteum is considered good evidence of current ovulation.
If tubal recanalization surgery is planned, it is a good idea to perform a preliminary laparoscopy to asses the prospect of the successful anastomosis. If the length of the remaining tube is less than 2 cm the recanalization surgery should not be attempted and IVF should be tried.
An ovarian biopsy can also be taken at the time of diagnostic laparoscopy to diagnose the cause of amenorrhea and infertility. Although the functional test of ovarian stimulation by a gonadotropin-releasing hormone is more in use it can be still of help if the presence of primordial follicles is in doubt in primary amenorrhea or premature ovarian failure.
Contraindications
Contraindications may include:
• Hemodynamic instability
• Mechanical or paralytic ileus
• Uncorrected coagulopathy
• Generalized peritonitis
• Severe cardiopulmonary disease
• Abdominal wall infection
• Multiple previous abdominal procedures
• Late pregnancy.
However, the final decision is determined not only by the clinical condition of patients but also by the surgeon’s judgment.
Choice of Anesthesia
Diagnostic laparoscopy can be performed under local anesthesia. Sedation with diazepam and pethidine can be used to make the patient unaware of a procedure because an unpleasant sensation of stretching of peritoneum due to pneumoperitoneum cannot be abolished by local anesthesia. Local anesthetic four percent Xylocaine can be injected subcutaneously over the inferior crease of the umbilicus.

Local anesthesia can be used for diagnostic laparoscopy
Epidural anesthesia is not liked by many anesthetists because anesthetizing the entire peritoneum high block is necessary and it would interfere with intercostal nerves and respiration will be affected. General anesthesia with good muscle relaxation is ideal in laparoscopic surgery.
Laparoscopic Anatomy
Diagnostic laparoscopy can be necessary for many undiagnosed surgical problems and knowledge of the laparoscopic anatomy of the whole abdomen is necessary. However, the most common indication of diagnostic laparoscopy is gynecological and especially infertility.
From anterior to posterior, the following important tubular structures are found crossing the brim of the true pelvis. The round ligament of the uterus, the infundibulopelvic ligament, which contains the gonadal vessels and the ureter. The ovaries and fallopian tubes are found between the round ligament and the infundibulopelvic ligament. The fallopian tubes arise from the superior portion of the uterus just above the attachment points of the round ligament. Laparoscopically, the round ligaments overhang the fallopian tube because of uterine manipulation and can be easily mistaken for them. The fallopian tubes towards their lateral end encircle the ovaries partially with their fimbriated ends. If the uterus deviates to the contralateral side with the help of uterine manipulator infundibulopelvic ligament is spread out and a pelvic sidewall triangle is created. The base of this triangle is the round ligament, the medial side is the infundibulopelvic ligament, and the lateral side is the external iliac artery. The apex of this triangle is the point at which the infundibulopelvic ligament crosses the external iliac artery.
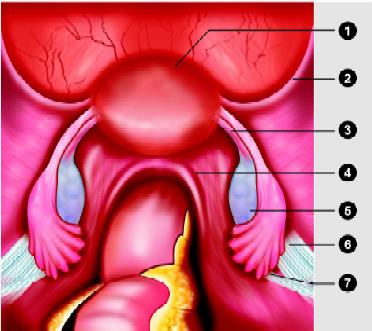
Laparoscopic anatomy of the normal pelvis: (1) Uterus; (2) Round ligament; (3) Utero-ovarian ligament (proper ovarian ligament); (4) Uterosacral ligament; (5) Ovary; (6) Suspensory ligament of the ovary; (7) Ureter

Anatomy of adnexa
Patient Position
The anesthetized patient is placed on the operating table with the legs straight or lithotomy position if female. The lithotomy position will allow the gynecologists and assistant to work simultaneously and uterine manipulation would be possible. The thighs must not be flexed onto the abdominal wall as they would be in the full lithotomy position used for other open surgical gynecological procedures. The operating table is tilted head up or down by approximately 15° depending on the main area of examination. Compression bandage may be used on the leg during the operation to prevent thromboembolism especially if a patient is in the lithotomy position.
Position of the Surgical Team
Before starting diagnostic laparoscopy the best guess is made about the quadrant in which pathology is likely to be found. The surgeon should stand opposed to this quadrant to allow a direct view into this quadrant. If the pathology is more likely in the pelvic cavity the surgeon stands on the left side of the patient. The first assistant, whose main task is to position the video camera, is also on the patient's left side. The instrument trolley is placed on the patient's left, allowing the scrub nurse to assist with placing the appropriate instruments in the operating ports. Television monitors are positioned on either side of the top end of the operating table at a suitable height for surgeon, anesthetists, as well as assistant to see the procedure.
Port Position
Generally, one optical port in umbilicus and one 5 mm port in left iliac fossa is required. Some gynecologists put their second port in the suprapubic region in the midline. In our opinion, the left iliac fossa port is better because it gives an elevation angle of 30° and the manipulation angle of 60°, which is ergonomically better. With suprapubic port elevation angle of the instrument and tubal structure is 90° and hence lifting up of ovary and tube may be difficult without grasping it. During a diagnostic laparoscopy, it is advisable that both telescope and the probing instrument is held by the surgeon himself as he knows better what he wants to see and where he wants to concentrate more and which structure he wants to see in a magnified close-up view. At the time of diagnostic laparoscopy, the surgeon should try to be very gentle with the tubal structure and bowel so that adhesion will not form and the stricture of the tube will not occur. Viewing of lateral pelvic organs is helped by the manipulation of mobile structure with a second port introduced through the left iliac fossa port. Many gynecologists introduce the second port in the suprapubic region but the elevation angle of the instrument is 90° and the mobilization of organs is difficult. A three-port approach should be used if there is any difficulty in manipulation with two ports especially in case of extensive adhesion.
• 10 mm umbilical (optical)
• 5 mm suprapubic
• 5 mm right hypochondrium.
A 30° telescope is employed in most instances, as this facilitates easier inspection of the deeper peritoneal cavity and abdominal organs. The secondary ports are inserted under laparoscopic vision. The selected site on the abdominal wall is identified by finger indentation of the parietal peritoneum.
The optimum incision is in the sub umbilical region. The open technique for trocar insertion is recommended if a patient presents with severe abdominal distension. Nitrous oxide is used if diagnostic laparoscopy is performed in local anesthesia because nitrous oxide has its own analgesic effect. Carbon dioxide is the preferred gas if diagnostic laparoscopy is performed under general anesthesia. Insufflation should be very slow and with care taken not to exceed 12.0 mm Hg.
Operative Procedure
The first step in diagnostic laparoscopy is a thorough exploration, just as during exploratory laparotomy. A systematic approach to exploration is essential to ensure that nothing is missed.
Systemic Plan of Inspection in Mid Abdomen
Positioning is the primary means of displacing the bowel and exposing peritoneal surfaces. In women with a deep pelvis, the bowel should be displaced gently into the upper abdomen, using a blunt probe or closed blunt grasping instrument to avoid laceration of the bowel or mesentery. An additional port with a blunt-tipped instrument may be used. Occasionally, a fan retractor should be used to retract full sigmoid colon. This instrument can be inserted through a 5 mm trocar cannula and fanned out in the abdomen to retract the bowel. Some common findings are shown.

Bicornuate uterus

Polycystic ovary
Inspection of Pelvis
The patient should again be positioned in steep Trendelenburg’s position. After assessing the genital organs, the gynecologist may wish to view areas outside the pelvis. This should be done by tilting the table head up or laterally to examine the paracolic or sub-diaphragmatic spaces.
Role of Laparoscopy in Ascites
Although the determination of the etiology of ascites is usually straight forward by history, physical examination, and analysis of ascitic fluid, the diagnosis of tuberculous or carcinomatous ascites may be elusive. In such cases, laparoscopy with biopsy is highly accurate. Peritoneal mesothelioma is frequently missed on the ascitic fluid by cytology and by blind biopsy. This entity is readily diagnosed by laparoscopy with peritoneal biopsy. Laparoscopy may be useful in the evaluation of hepatic malignancy (either primary or metastatic). Eighty percent to 90 percent of these lesions are present on the hepatic surface and up to 2/3 of the liver surface may be inspected by laparoscopy. When a surgical resection is a therapeutic option, laparoscopy may reveal small (1 cm or less) metastatic lesions, peritoneal metastases, or cirrhosis, which represent contraindications to resection and are frequently missed on CT, MRI, and the US. The use of laparoscopic ultrasound allows the detection of deeper lesions and vascular infiltration.
In studying the role of laparoscopy in the diagnosis and differential diagnosis of ascites out of 2,500 patients who underwent laparoscopy 30.89 percent had ascites; liver cirrhosis underlays it in 57.78 percent, peritoneal carcinosis in 26.29 percent, primary and metastatic carcinoma in 12.95 percent, tuberculous peritonitis in 1.42 percent, more rarely other diseases. Liver cirrhosis, malignant tumors, and the other hepatic affections with concomitant ascites in their course can certainly be diagnosed laparoscopically. Laparoscopy with oriented biopsy of peritoneum and liver is of decisive importance in differentiating peritoneal carcinosis from tuberculosis. In peritoneal carcinosis, the diagnosis (as based in clinical and laboratory findings) coincided perfectly with the laparoscopic and histologic one in 24.5 percent, partially in 45.5 percent. In 30 percent there was no congruence at all. Laparoscopy and the test methods associated with it contributed to the accurate diagnosis of peritoneal carcinosis in 75.5 percent of the patients. Ovarian carcinoma (20.9%) and cancer of the stomach (16.3%) underlay peritoneal carcinosis most frequently, other diseases by far more seldom.
Diagnostic peritoneoscopies was performed in 226 patients with ascites. A satisfactory examination was possible in 220 patients. The clinical diagnosis was confirmed at peritoneoscopy in 82.7 percent of patients. Peritoneoscopic examination corrected the clinical diagnosis in 13.7 percent, was inconclusive in 2.6 percent, and was incorrect in 0.8 percent of cases. It was 100 percent diagnostic in malignant peritonitis and 89.5 percent in patients with tuberculous peritonitis. Pseudomyxoma peritoneal and mesothelioma was suspected in one patient each at peritoneoscopy and was confirmed histologically. The utility of routine ascitic fluid examination was reviewed in all patients. The ascitic fluid was transudative in 81.9 percent, exudative in 8.6 percent, and indeterminate in 9.5 percent of patients with cirrhosis of the liver. Patients with tuberculous peritonitis had exudative, transudative, and indeterminate ascites in 71.8 percent, 3.2 percent, and 25 percent respectively. The ascites in patients with malignant peritonitis was either exudative (80%) or indeterminate (20%). There was considerable overlap in the nature of ascites present in the three groups of patients. We, therefore, conclude that peritoneoscopy is the most valuable investigation in the diagnosis of ascites, particularly in exudative and indeterminate types.
The Value of Laparoscopic Diagnosis of TB
The laparoscopic and pathological diagnoses of 43 patients who underwent abdominal laparoscopy for various indications are presented. Major indications for the laparoscopy included hepatomegaly in 32 patients, ascites in 28, and pyrexia of unknown origin (PUO) in 18 patients. A combination of two or more of these indications was a more common feature. The most frequently encountered laparoscopic diagnoses were tuberculosis and chronic liver disease (16 patients each), followed by cancer (9 patients). However, on pathological examination of peritoneal or liver biopsy tissue and on follow-up, tuberculosis was confirmed in 12 patients, chronic liver disease in 14 patients, and hepatocellular carcinoma in 11 patients. No complications were encountered during the laparoscopy. Our findings indicate that abdominal laparoscopy is a safe, quick, and inexpensive diagnostic tool, particularly when appropriate and adequate tissue is taken for pathological examination. In such instances, laparoscopy would save an unnecessary laparotomy, especially where tuberculosis and cancer are considered in the differential diagnosis.
Due to its high accuracy, some suggest PCR before laparoscopy. In the light of our accumulated experience, we would suggest that PCR of ascetic fluid obtained by US-guided fine-needle aspiration is now the investigation of choice for patients with the described clinical and radiological presentations and should at least be attempted before surgical intervention. If the result is negative, diagnostic laparoscopy, or, if this is not feasible, laparotomy should be performed.
Role of Laparoscopy in Carcinoma Assessment
A pretherapeutic staging system to design operative or neoadjuvant treatments in gastric cancer is needed. It can be done under local anesthesia sensitive predictor of peritoneal recurrence. Staging laparoscopy with peritoneal lavage cytology is a safe, effective tool in patients with locally advanced gastric cancer, especially in patients receiving neoadjuvant chemotherapy. The ability of minimally invasive surgeons and endoscopists to diagnose and palliate unrespectable pancreatic cancer is likely to continue to improve and these techniques will play an increasingly important role in the care of patients with pancreatic cancer. Likewise, the accuracy of radiological imaging techniques to detect unre- spectable disease will also continue to advance and further decrease the incidence of nontherapeutic laparotomies. It is valuable in many therapeutic uses as in staging of the tumor, catheter placement in nephrogenic ascites.
Dialysis Catheter and Laparoscopy
Regarding complications of dialysis catheter insertion Tiong reported surgical early and late complications of a dialysis catheter. Of open Tenckhoff catheter insertion under local anesthesia in a single institution. A review was carried out on 164 insertions in 139 patients over a three-year period. Tenckhoff catheter insertion for CAPD is a procedure associated with significant surgical morbidity. Patients with diabetes mellitus, glomerulonephritis, and ongoing sepsis are at greater risk of early complications, and hence, must have their conditions stabilized or treated before surgery. In addition, prolonged surgical time and patients with previous abdominal surgery are at increased risk. The rate of complications may be improved by early consideration of patients with poor tolerance of local anesthetic surgery or with previous abdominal surgery for laparoscopic insertion under general anesthesia. To prevent late complications dominated by CAPD peritonitis, the patient’s nutritional status and care of the catheter should both be optimized.
Open insertion of peritoneal dialysis (PD) catheters is the standard surgical technique, but it is associated with a relatively high incidence of catheter outflow obstruction and dialysis leak. Omental wrapping is the most common cause of the mechanical problems; the laparoscopic omental fixation technique is of higher value in addition to laparoscopic surgery also enabled diagnosis of intra-abdominal pathologies and treatment of the accompanying surgical problems during the same operation.
Port-site Metastasis
The risk of port-site metastases in those undergoing laparoscopy for gynecologic malignancy was highest in those with ascites in a study of 82 patients. The study participants underwent 87 procedures that involved 330 trocar sites. The overall risk of port-site metastases per procedure was 2.3 percent, and per port, the site was 2.4 percent, Dr. Nimesh Nagarsheth, at an international congress sponsored by the Society of Laparoendoscopic Surgeons reported 39 patients with endometrial cancer, 29 with ovarian cancer, and 14 with cervical cancer. Twenty of those were treated for recurrent cancer, and 10 had ascites. They were followed for an average of 361 days. Port-site metastases occurred in two patients. The first developed metastases at five sites, and was diagnosed 13 days after second-look laparoscopy for stage IIIB ovarian cancer. The second had metastases at three sites and was diagnosed 46 days after second-look laparoscopy for stage IIIC primary peritoneal cancer. Both patients had ascites.
Laparoscopy and Ascites
Laparoscopy in ascites is a safe and cost-effective diagnostic modality and its rules extended the diagnostic procedure providing in the unexplained cause of ascites definitive diagnosis. In such instances, laparoscopy would save an unnecessary laparotomy; especially where tuberculosis and cancer are considered in the differential diagnosis.
Diagnostic Laparoscopy
The usual site of insertion of the trocar/cannula for diagnostic laparoscopy is below or to the side of the umbilicus. This position may require to be altered in the presence of abdominal scars. The use of a 30° forward oblique telescope is preferable for viewing the surface architecture of organs. By rotation of the telescope, different angles of inspection can be achieved.
The first important step after access to the abdomen has been gained, is to check for damage caused by trocar insertion. A second 5 mm port may then be inserted under vision in an appropriate quadrant to take a palpating rod. A systematic examination of the abdomen must be performed just as in laparotomy. We begin at the left lobe of the liver but any scheme can be used as long as it is consistent. Next, check around the falciform ligament to the right lobe of the liver, gallbladder, and hiatus. After checking the stomach, move onto the cecum and appendix and check the terminal ileum. Follow the colon round to the sigmoid colon, and then check the pelvis. The surgeon should be conversant with sampling and biopsy techniques, the use of position and manipulation to aid vision.
At the time of diagnostic laparoscopy, all the abdominal organs are inspected for any gross anatomical abnormalities. The abdominal cavity is inspected for an excess of fluids. Samples are taken if the free fluid is present for laboratory tests (chemistry, cytology, or bacteriology). Peritoneal lavage and adhesiolysis may need to be performed to improve the visualization of organs. At the time of peritoneal lavage when fluid is sucked from the cul-de-sac, it is important to keep all the holes of the suction-irrigator beneath the level of the fluid to avoid removing pneumoperitoneum. If the suction-irrigator is positioned improperly, the CO2 gas will be removed preferentially. However, with high-flow insufflators, pneumoperitoneum rarely is lost and quickly restored.
When performing a diagnostic laparoscopy to confirm appendicitis, a 5 mm port is placed in the left iliac fossa to facilitate manipulation. The patient is placed head down and rotated to the left to displace the small bowel from the pelvis and allow the uterus and ovaries to be checked. This, however, should be limited to avoid contamination of subphrenic spaces, if this is not already present.
Ending of the Operation
During a diagnostic laparoscopy, the surgeon can perform therapeutic laparoscopy if indicated and consent from a patient’s relative can be obtained. At the end of the surgery, the abdomen should be re-examined for any possible bowel injury or hemorrhage. The entire accessory instrument and then the port is removed. The telescope should be removed leaving gas valve of umbilical port open to let out all the gas. Once the complete gas is out, removing the primary cannula telescope or any blunt instrument should be introduced again and cannula should be pulled over that instrument to prevent pull of omentum or bowel. The wound should be closed with suture. Vicryl should be used for rectus and un-absorbable intradermal or stapler for the skin. Only a 10 mm port wound is necessary to repair. Adhesive sterile dressing over the wound should be applied.
A patient may be discharged on the same day after an operation if everything goes well. The patient may have slight pain initially but usually resolves. Diagnostic laparoscopy is a useful method for reducing hospital stay, complications, and return to normal activity if carried on in a proper manner.
Diagnostic laparoscopy is a minimally invasive surgical procedure that allows the visual examination of intraabdominal organs in order to detect pathology. The procedure allows the direct visual examination of intraabdominal organs including large surface areas of the liver, gallbladder, spleen, peritoneum, pelvic organs, and retroperitoneum. Biopsies, aspiration, and cultures can be obtained, and laparoscopic ultrasound may be used.
Diagnostic laparoscopy is safe and well-tolerated and can be performed in an outpatient or inpatient setting under general anesthesia. There may also be unique circumstances where office-based diagnostic laparoscopy may be considered under local anesthesia. These circumstances should include only procedures where complications and the need for therapeutic procedures through the same access are extremely unlikely. Manipulation and biopsy of the viscera are possible through additional ports. Diagnostic laparoscopy is the most commonly performed gynecological procedure today. Its greatest advantage is that it has replaced exploratory laparotomy.
Diagnostic laparoscopy was first introduced in 1901, when Kelling, performed a peritoneoscopy in a dog and was called ‘‘celioscopy’’. A Swedish internist named Jacobaeusc is credited with performing the first diagnostic laparoscopy on humans in 1910. He described its application in patients with ascites and for the early diagnosis of malignant lesions. In the last ten years, laparoscopy has made a great difference to the diagnosis of abdominal acute and chronic pain. It has evolved as an informative important method of diagnosing a wide spectrum of both benign and malignant diseases. Elective diagnostic laparoscopy refers to the use of the procedure in chronic intra-abdominal disorders. Emergency diagnostic laparoscopy is performed in patients presenting with an acute abdomen.
Indications
The indications for diagnostic laparoscopy can be divided into two main groups.
Non-traumatic, Non-gynecological Acute Abdomen Like:
• Appendicitis
• Diverticulitis
• Duodenal perforation
• Mesenteric adenitis
• Intestinal adhesion
• Omental necrosis
• Intestinal infarction
• Complicated Meckel’s diverticulum
• Bedside laparoscopy in the ICU
• Torsion of the intra-abdominal testis.
Gynecological Abdominal Emergencies Like:
• Ovarian cysts
• Pelvic inflammatory diseases
• Acute salpingitis
• Ectopic pregnancy
• Endometriosis
• Perforated uterus due to criminal abortion
• Salpingitis.
One of the important uses for diagnostic laparoscopy is the investigation of female infertility. Tubal causes of infertility are found in 15 percent of a couple. In these patients, laparoscopy not only allows tubal patency to be assessed but also enables other features in the pelvis to be examined. The most important findings related to infertility are kinking of the tube, fimbrial damage, or ovarian adhesions. The presence of corpus luteum is considered good evidence of current ovulation.
If tubal recanalization surgery is planned, it is a good idea to perform a preliminary laparoscopy to asses the prospect of the successful anastomosis. If the length of the remaining tube is less than 2 cm the recanalization surgery should not be attempted and IVF should be tried.
An ovarian biopsy can also be taken at the time of diagnostic laparoscopy to diagnose the cause of amenorrhea and infertility. Although the functional test of ovarian stimulation by a gonadotropin-releasing hormone is more in use it can be still of help if the presence of primordial follicles is in doubt in primary amenorrhea or premature ovarian failure.
Contraindications
Contraindications may include:
• Hemodynamic instability
• Mechanical or paralytic ileus
• Uncorrected coagulopathy
• Generalized peritonitis
• Severe cardiopulmonary disease
• Abdominal wall infection
• Multiple previous abdominal procedures
• Late pregnancy.
However, the final decision is determined not only by the clinical condition of patients but also by the surgeon’s judgment.
Choice of Anesthesia
Diagnostic laparoscopy can be performed under local anesthesia. Sedation with diazepam and pethidine can be used to make the patient unaware of a procedure because an unpleasant sensation of stretching of peritoneum due to pneumoperitoneum cannot be abolished by local anesthesia. Local anesthetic four percent Xylocaine can be injected subcutaneously over the inferior crease of the umbilicus.

Local anesthesia can be used for diagnostic laparoscopy
Epidural anesthesia is not liked by many anesthetists because anesthetizing the entire peritoneum high block is necessary and it would interfere with intercostal nerves and respiration will be affected. General anesthesia with good muscle relaxation is ideal in laparoscopic surgery.
Laparoscopic Anatomy
Diagnostic laparoscopy can be necessary for many undiagnosed surgical problems and knowledge of the laparoscopic anatomy of the whole abdomen is necessary. However, the most common indication of diagnostic laparoscopy is gynecological and especially infertility.
From anterior to posterior, the following important tubular structures are found crossing the brim of the true pelvis. The round ligament of the uterus, the infundibulopelvic ligament, which contains the gonadal vessels and the ureter. The ovaries and fallopian tubes are found between the round ligament and the infundibulopelvic ligament. The fallopian tubes arise from the superior portion of the uterus just above the attachment points of the round ligament. Laparoscopically, the round ligaments overhang the fallopian tube because of uterine manipulation and can be easily mistaken for them. The fallopian tubes towards their lateral end encircle the ovaries partially with their fimbriated ends. If the uterus deviates to the contralateral side with the help of uterine manipulator infundibulopelvic ligament is spread out and a pelvic sidewall triangle is created. The base of this triangle is the round ligament, the medial side is the infundibulopelvic ligament, and the lateral side is the external iliac artery. The apex of this triangle is the point at which the infundibulopelvic ligament crosses the external iliac artery.
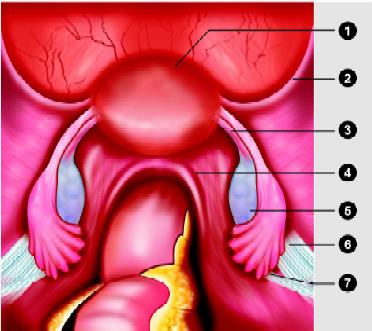
Laparoscopic anatomy of the normal pelvis: (1) Uterus; (2) Round ligament; (3) Utero-ovarian ligament (proper ovarian ligament); (4) Uterosacral ligament; (5) Ovary; (6) Suspensory ligament of the ovary; (7) Ureter

Anatomy of adnexa
Patient Position
The anesthetized patient is placed on the operating table with the legs straight or lithotomy position if female. The lithotomy position will allow the gynecologists and assistant to work simultaneously and uterine manipulation would be possible. The thighs must not be flexed onto the abdominal wall as they would be in the full lithotomy position used for other open surgical gynecological procedures. The operating table is tilted head up or down by approximately 15° depending on the main area of examination. Compression bandage may be used on the leg during the operation to prevent thromboembolism especially if a patient is in the lithotomy position.
Position of the Surgical Team
Before starting diagnostic laparoscopy the best guess is made about the quadrant in which pathology is likely to be found. The surgeon should stand opposed to this quadrant to allow a direct view into this quadrant. If the pathology is more likely in the pelvic cavity the surgeon stands on the left side of the patient. The first assistant, whose main task is to position the video camera, is also on the patient's left side. The instrument trolley is placed on the patient's left, allowing the scrub nurse to assist with placing the appropriate instruments in the operating ports. Television monitors are positioned on either side of the top end of the operating table at a suitable height for surgeon, anesthetists, as well as assistant to see the procedure.
Port Position
Generally, one optical port in umbilicus and one 5 mm port in left iliac fossa is required. Some gynecologists put their second port in the suprapubic region in the midline. In our opinion, the left iliac fossa port is better because it gives an elevation angle of 30° and the manipulation angle of 60°, which is ergonomically better. With suprapubic port elevation angle of the instrument and tubal structure is 90° and hence lifting up of ovary and tube may be difficult without grasping it. During a diagnostic laparoscopy, it is advisable that both telescope and the probing instrument is held by the surgeon himself as he knows better what he wants to see and where he wants to concentrate more and which structure he wants to see in a magnified close-up view. At the time of diagnostic laparoscopy, the surgeon should try to be very gentle with the tubal structure and bowel so that adhesion will not form and the stricture of the tube will not occur. Viewing of lateral pelvic organs is helped by the manipulation of mobile structure with a second port introduced through the left iliac fossa port. Many gynecologists introduce the second port in the suprapubic region but the elevation angle of the instrument is 90° and the mobilization of organs is difficult. A three-port approach should be used if there is any difficulty in manipulation with two ports especially in case of extensive adhesion.
• 10 mm umbilical (optical)
• 5 mm suprapubic
• 5 mm right hypochondrium.
A 30° telescope is employed in most instances, as this facilitates easier inspection of the deeper peritoneal cavity and abdominal organs. The secondary ports are inserted under laparoscopic vision. The selected site on the abdominal wall is identified by finger indentation of the parietal peritoneum.
The optimum incision is in the sub umbilical region. The open technique for trocar insertion is recommended if a patient presents with severe abdominal distension. Nitrous oxide is used if diagnostic laparoscopy is performed in local anesthesia because nitrous oxide has its own analgesic effect. Carbon dioxide is the preferred gas if diagnostic laparoscopy is performed under general anesthesia. Insufflation should be very slow and with care taken not to exceed 12.0 mm Hg.
Operative Procedure
The first step in diagnostic laparoscopy is a thorough exploration, just as during exploratory laparotomy. A systematic approach to exploration is essential to ensure that nothing is missed.
Systemic Plan of Inspection in Mid Abdomen
Positioning is the primary means of displacing the bowel and exposing peritoneal surfaces. In women with a deep pelvis, the bowel should be displaced gently into the upper abdomen, using a blunt probe or closed blunt grasping instrument to avoid laceration of the bowel or mesentery. An additional port with a blunt-tipped instrument may be used. Occasionally, a fan retractor should be used to retract full sigmoid colon. This instrument can be inserted through a 5 mm trocar cannula and fanned out in the abdomen to retract the bowel. Some common findings are shown.

Bicornuate uterus

Polycystic ovary
Inspection of Pelvis
The patient should again be positioned in steep Trendelenburg’s position. After assessing the genital organs, the gynecologist may wish to view areas outside the pelvis. This should be done by tilting the table head up or laterally to examine the paracolic or sub-diaphragmatic spaces.
Role of Laparoscopy in Ascites
Although the determination of the etiology of ascites is usually straight forward by history, physical examination, and analysis of ascitic fluid, the diagnosis of tuberculous or carcinomatous ascites may be elusive. In such cases, laparoscopy with biopsy is highly accurate. Peritoneal mesothelioma is frequently missed on the ascitic fluid by cytology and by blind biopsy. This entity is readily diagnosed by laparoscopy with peritoneal biopsy. Laparoscopy may be useful in the evaluation of hepatic malignancy (either primary or metastatic). Eighty percent to 90 percent of these lesions are present on the hepatic surface and up to 2/3 of the liver surface may be inspected by laparoscopy. When a surgical resection is a therapeutic option, laparoscopy may reveal small (1 cm or less) metastatic lesions, peritoneal metastases, or cirrhosis, which represent contraindications to resection and are frequently missed on CT, MRI, and the US. The use of laparoscopic ultrasound allows the detection of deeper lesions and vascular infiltration.
In studying the role of laparoscopy in the diagnosis and differential diagnosis of ascites out of 2,500 patients who underwent laparoscopy 30.89 percent had ascites; liver cirrhosis underlays it in 57.78 percent, peritoneal carcinosis in 26.29 percent, primary and metastatic carcinoma in 12.95 percent, tuberculous peritonitis in 1.42 percent, more rarely other diseases. Liver cirrhosis, malignant tumors, and the other hepatic affections with concomitant ascites in their course can certainly be diagnosed laparoscopically. Laparoscopy with oriented biopsy of peritoneum and liver is of decisive importance in differentiating peritoneal carcinosis from tuberculosis. In peritoneal carcinosis, the diagnosis (as based in clinical and laboratory findings) coincided perfectly with the laparoscopic and histologic one in 24.5 percent, partially in 45.5 percent. In 30 percent there was no congruence at all. Laparoscopy and the test methods associated with it contributed to the accurate diagnosis of peritoneal carcinosis in 75.5 percent of the patients. Ovarian carcinoma (20.9%) and cancer of the stomach (16.3%) underlay peritoneal carcinosis most frequently, other diseases by far more seldom.
Diagnostic peritoneoscopies was performed in 226 patients with ascites. A satisfactory examination was possible in 220 patients. The clinical diagnosis was confirmed at peritoneoscopy in 82.7 percent of patients. Peritoneoscopic examination corrected the clinical diagnosis in 13.7 percent, was inconclusive in 2.6 percent, and was incorrect in 0.8 percent of cases. It was 100 percent diagnostic in malignant peritonitis and 89.5 percent in patients with tuberculous peritonitis. Pseudomyxoma peritoneal and mesothelioma was suspected in one patient each at peritoneoscopy and was confirmed histologically. The utility of routine ascitic fluid examination was reviewed in all patients. The ascitic fluid was transudative in 81.9 percent, exudative in 8.6 percent, and indeterminate in 9.5 percent of patients with cirrhosis of the liver. Patients with tuberculous peritonitis had exudative, transudative, and indeterminate ascites in 71.8 percent, 3.2 percent, and 25 percent respectively. The ascites in patients with malignant peritonitis was either exudative (80%) or indeterminate (20%). There was considerable overlap in the nature of ascites present in the three groups of patients. We, therefore, conclude that peritoneoscopy is the most valuable investigation in the diagnosis of ascites, particularly in exudative and indeterminate types.
The Value of Laparoscopic Diagnosis of TB
The laparoscopic and pathological diagnoses of 43 patients who underwent abdominal laparoscopy for various indications are presented. Major indications for the laparoscopy included hepatomegaly in 32 patients, ascites in 28, and pyrexia of unknown origin (PUO) in 18 patients. A combination of two or more of these indications was a more common feature. The most frequently encountered laparoscopic diagnoses were tuberculosis and chronic liver disease (16 patients each), followed by cancer (9 patients). However, on pathological examination of peritoneal or liver biopsy tissue and on follow-up, tuberculosis was confirmed in 12 patients, chronic liver disease in 14 patients, and hepatocellular carcinoma in 11 patients. No complications were encountered during the laparoscopy. Our findings indicate that abdominal laparoscopy is a safe, quick, and inexpensive diagnostic tool, particularly when appropriate and adequate tissue is taken for pathological examination. In such instances, laparoscopy would save an unnecessary laparotomy, especially where tuberculosis and cancer are considered in the differential diagnosis.
Due to its high accuracy, some suggest PCR before laparoscopy. In the light of our accumulated experience, we would suggest that PCR of ascetic fluid obtained by US-guided fine-needle aspiration is now the investigation of choice for patients with the described clinical and radiological presentations and should at least be attempted before surgical intervention. If the result is negative, diagnostic laparoscopy, or, if this is not feasible, laparotomy should be performed.
Role of Laparoscopy in Carcinoma Assessment
A pretherapeutic staging system to design operative or neoadjuvant treatments in gastric cancer is needed. It can be done under local anesthesia sensitive predictor of peritoneal recurrence. Staging laparoscopy with peritoneal lavage cytology is a safe, effective tool in patients with locally advanced gastric cancer, especially in patients receiving neoadjuvant chemotherapy. The ability of minimally invasive surgeons and endoscopists to diagnose and palliate unrespectable pancreatic cancer is likely to continue to improve and these techniques will play an increasingly important role in the care of patients with pancreatic cancer. Likewise, the accuracy of radiological imaging techniques to detect unre- spectable disease will also continue to advance and further decrease the incidence of nontherapeutic laparotomies. It is valuable in many therapeutic uses as in staging of the tumor, catheter placement in nephrogenic ascites.
Dialysis Catheter and Laparoscopy
Regarding complications of dialysis catheter insertion Tiong reported surgical early and late complications of a dialysis catheter. Of open Tenckhoff catheter insertion under local anesthesia in a single institution. A review was carried out on 164 insertions in 139 patients over a three-year period. Tenckhoff catheter insertion for CAPD is a procedure associated with significant surgical morbidity. Patients with diabetes mellitus, glomerulonephritis, and ongoing sepsis are at greater risk of early complications, and hence, must have their conditions stabilized or treated before surgery. In addition, prolonged surgical time and patients with previous abdominal surgery are at increased risk. The rate of complications may be improved by early consideration of patients with poor tolerance of local anesthetic surgery or with previous abdominal surgery for laparoscopic insertion under general anesthesia. To prevent late complications dominated by CAPD peritonitis, the patient’s nutritional status and care of the catheter should both be optimized.
Open insertion of peritoneal dialysis (PD) catheters is the standard surgical technique, but it is associated with a relatively high incidence of catheter outflow obstruction and dialysis leak. Omental wrapping is the most common cause of the mechanical problems; the laparoscopic omental fixation technique is of higher value in addition to laparoscopic surgery also enabled diagnosis of intra-abdominal pathologies and treatment of the accompanying surgical problems during the same operation.
Port-site Metastasis
The risk of port-site metastases in those undergoing laparoscopy for gynecologic malignancy was highest in those with ascites in a study of 82 patients. The study participants underwent 87 procedures that involved 330 trocar sites. The overall risk of port-site metastases per procedure was 2.3 percent, and per port, the site was 2.4 percent, Dr. Nimesh Nagarsheth, at an international congress sponsored by the Society of Laparoendoscopic Surgeons reported 39 patients with endometrial cancer, 29 with ovarian cancer, and 14 with cervical cancer. Twenty of those were treated for recurrent cancer, and 10 had ascites. They were followed for an average of 361 days. Port-site metastases occurred in two patients. The first developed metastases at five sites, and was diagnosed 13 days after second-look laparoscopy for stage IIIB ovarian cancer. The second had metastases at three sites and was diagnosed 46 days after second-look laparoscopy for stage IIIC primary peritoneal cancer. Both patients had ascites.
Laparoscopy and Ascites
Laparoscopy in ascites is a safe and cost-effective diagnostic modality and its rules extended the diagnostic procedure providing in the unexplained cause of ascites definitive diagnosis. In such instances, laparoscopy would save an unnecessary laparotomy; especially where tuberculosis and cancer are considered in the differential diagnosis.
Diagnostic Laparoscopy
The usual site of insertion of the trocar/cannula for diagnostic laparoscopy is below or to the side of the umbilicus. This position may require to be altered in the presence of abdominal scars. The use of a 30° forward oblique telescope is preferable for viewing the surface architecture of organs. By rotation of the telescope, different angles of inspection can be achieved.
The first important step after access to the abdomen has been gained, is to check for damage caused by trocar insertion. A second 5 mm port may then be inserted under vision in an appropriate quadrant to take a palpating rod. A systematic examination of the abdomen must be performed just as in laparotomy. We begin at the left lobe of the liver but any scheme can be used as long as it is consistent. Next, check around the falciform ligament to the right lobe of the liver, gallbladder, and hiatus. After checking the stomach, move onto the cecum and appendix and check the terminal ileum. Follow the colon round to the sigmoid colon, and then check the pelvis. The surgeon should be conversant with sampling and biopsy techniques, the use of position and manipulation to aid vision.
At the time of diagnostic laparoscopy, all the abdominal organs are inspected for any gross anatomical abnormalities. The abdominal cavity is inspected for an excess of fluids. Samples are taken if the free fluid is present for laboratory tests (chemistry, cytology, or bacteriology). Peritoneal lavage and adhesiolysis may need to be performed to improve the visualization of organs. At the time of peritoneal lavage when fluid is sucked from the cul-de-sac, it is important to keep all the holes of the suction-irrigator beneath the level of the fluid to avoid removing pneumoperitoneum. If the suction-irrigator is positioned improperly, the CO2 gas will be removed preferentially. However, with high-flow insufflators, pneumoperitoneum rarely is lost and quickly restored.
When performing a diagnostic laparoscopy to confirm appendicitis, a 5 mm port is placed in the left iliac fossa to facilitate manipulation. The patient is placed head down and rotated to the left to displace the small bowel from the pelvis and allow the uterus and ovaries to be checked. This, however, should be limited to avoid contamination of subphrenic spaces, if this is not already present.
Ending of the Operation
During a diagnostic laparoscopy, the surgeon can perform therapeutic laparoscopy if indicated and consent from a patient’s relative can be obtained. At the end of the surgery, the abdomen should be re-examined for any possible bowel injury or hemorrhage. The entire accessory instrument and then the port is removed. The telescope should be removed leaving gas valve of umbilical port open to let out all the gas. Once the complete gas is out, removing the primary cannula telescope or any blunt instrument should be introduced again and cannula should be pulled over that instrument to prevent pull of omentum or bowel. The wound should be closed with suture. Vicryl should be used for rectus and un-absorbable intradermal or stapler for the skin. Only a 10 mm port wound is necessary to repair. Adhesive sterile dressing over the wound should be applied.
A patient may be discharged on the same day after an operation if everything goes well. The patient may have slight pain initially but usually resolves. Diagnostic laparoscopy is a useful method for reducing hospital stay, complications, and return to normal activity if carried on in a proper manner.


