Dr. Abdelgayoum Sulimen Basheir, MD. ABS, FRCS
Consultant urologist
Jubail General Hospital KSA
Member of Society International Urology
Member of Arab Society of Urology
Member of Arab Society of Andrology
Member of World Association of Laparoscopy (WALS)
Member of Sudanse Society of Surgery
Project submitted towards completion of Diploma in Minimal Access surgery at World Laparoscopy Hospital New Delhi , India , July 2008
Abstract
Ureteral injury during pelvic laparoscopic surgery is a known complication and it had morbidty depending on the time of their recognition. The incidence of these injuries are 0.5-2 % and most of these complications happened with gynaecology, endourology and general surgery operations. The risk factors precipating more injuries. Diagnosis of these injuries determine the out come, if diagnosed intraoperative repair should be done immediately. Late detection had bad morbidty and loss of some of renal functions. Ureteral injury can be prevented and reduced by more training and learning for surgeons and meticulous laparoscopic techniques. Laparoscopic ureteric injuries repair became popular by experience laparoscopy surgeon. Remute ureteral injury due to over cooking with the diathermy close to the ureter should be avoided.
Objective
The objective of this study was to review the literature in reference to deterrmine ureteral injury during laparoscopic surgery in pelvic operation to determine
- Rate of incidence
- Type of injury "thermal, tie ligation , transection"
- Location of the injury site
- Time of recognization "intraoperative, post operative"
- Mode of repair done
Material and methods
A literature search was performed using search engine Google and library facility available at Laparoscopic hospital in New Delhi and Springlink search. The following term were used in the reach ureteral injury, laparoscopic ureteral injuries, and laparoscopic pelvic surgery ureteral injury. Selected papers were screened for further references. Criteria for selection of the literature were number of cases less than twenty was excluded. Methods of analysis "statistical and non statistical". Operative procedure only universally accepted procedures and institution where the study was done specialized for laparoscopic surgeon.
Pelvic Anatomy
Schematic illustration of pelvic organs - anterior view

Schematic illustration of pelvic organs - lateral view
Risk Factors for Ureteric injury
- Limited experience of laparoscopic surgeon
- Intraoperative difficulties "bleeding"
- Past history of pelvic operation "adhesion"
- Excessive use of diathermy closed to Ureter
Common site of Ureteric injury is the lower third during
- Ligation of the uterine artery
- Lateral wall of the cervix dissection
- Utrosacral ligament dissection
- Dissection Close to iliac vessel bifurcation
- Abdomino perineum resection
Diagnosis of Ureteric injury
Immediate and early diagnosis determines the outcome following the injury.
Intra operative diagnosis
- Urinary leakage
- Intraoperative cystoscopy, retrograde
- Urteroscopy
- Intravenous urography
Delay diagnosis
- Clinically fever, flak pain, haematuria
- Ultrasound abdomen for collection, Hydronephrosis
- IVU- for extra vacation or complete obstruction\ C T- abdomen
Cystoscopy and retrograde help in diagnosis by detection of extravasation. While Urteroscopy visualized perforations. IVU Visualized any extravasation or obstruction due to suture tie. Ultrasound and CT abdomen detect any intra abdominal collection or hydronephrosis.
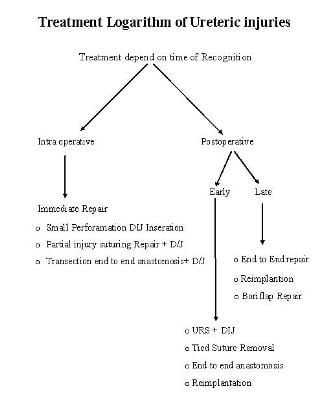
Surgical Treatment for Ureteric Injury depends on time of Recognition
A. Intra Operative: Immediate Repair should be done eg;
- Small Perforation - D/J
- Partial injury - Suturing
- Complete transection - Suturing and anastomosis end to end
B. Early detection treatment
- Urteroscopy + D/J insertion or Percutaneous Nephrostomy
- Suture tie Removal by Urteroscopy
- End to End anastomosis, Reimplantation Repair
C. Delayed detection treatment
- PCN and Bori flap
- Reimplantation of the Ureter
- Nephrectomy is if No other Choice
- Surgical repair of Ureteric injuries depend on time of diagnosis and experience of the operating surgeon who repair intraoperative injuries by laparoscopic or laparotomy .
- Simple injuries like small perforation are treated with D/J insertion. Partial and complete transection need exploration and repair by laparoscopy or laparotomy, suturing and end to end anastomosis .Late diagnosis cases may need end to end anastomosis, reimplantation, boriflap with or without PCN according to the condition.
Discussion
Revision of literature was done for ureteral injuries during laparoscopy pelvic surgery. The article revised was published by know centers and institute and universities incidence and risks factors and time of Recognition of the ureteral injury and type of repair done was the centre of discussion in all papers. In France Leonard frank study 1300 case post laparoscopic hysterectomy and concluded that rate of ureteral injuries was comparable to open hysterectomy and prevention of these complication by improving the surgeons experience. In another article Charles chaperon revised the laparoscopic complication of 29966 cases of pelvic laparoscopic surgeries for complication of surgery during laparoscopy and he stated awareness and good laparoscopic experience will prevent and reduce the complication and early diagnosis always followed by less morbidity and good out come. Raut.V, from Bombay made retrospective study for 296 case who had pelvic operation with complication injuries of 15 in urinary bladder and 2 in Ureter. Concluded awareness of gynaecology surgeon reduces the incidence of Ureteric injuries. Matani from Jordon revised 42 cases seen in his department with Ureteric injury following pelvic surgery. His research ended with the fact that early Ureteric injury discovered the better outcome. Adhout from France revised Ureteric injuries in his centre in 24 cases Reported during laparoscopy. He mentioned most of the injuries done by gynecology in pelvic surgery and time of detection is essential in the plan of treatment. Serglori from USA made his study in value of intra operative cystoscopy for all case of laparoscopic Hysterectomy and he found all injuries in his series which are 118 cases were detected intra operative and repair done in the same surgery so he recommended intra operative cystoscopy for laparoscopic hysterectomy specially in difficult cases. In all Papers 1/3 of the injuries discover intraoperative. This risk factor shared in most of the injuries. Recently the usage of fibreoptic Ureteric probe makes the identification of Ureters very easy during surgery specially in difficult cases.
Conclusion
- Awareness of Risk factors and good experience in laparoscopy are the main factors in preventing and reducing the Ureteric injuries.
- Immediate and early diagnosis of ureteral injuries gives excellent out come and minimal morbidty. While delayed diagnosis had prolong morbidity.
- For any suspicious of Ureteric injury investigation should be done to role out the injury.
- Placement of stent is helpful specially in difficult cases reduce rate of Ureteric injury.
- Intra operative cystoscopy during laparoscopy leads to immediate diagnosis of Ureteric injuries.
- Excessive use of diathermy near the Ureter follow by thermal injury
Reference:
- Carley ME, McIntire D, Carley JM, Schaffer J. Incidence, risk factors and morbidity of unintended bladder or ureter injury during hysterectomy. Int Urogynecol J Pelvic Floor Dysfunct (2002) 13:18-21
- Chapron C, Fauconnier A, Goffinet F, Bréart G, Dubuisson JB. Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynaecologic pathology. Results of a meta-analysis. Hum Reprod (2002) 17:1334-1342.
- Dandolu V, Mathai E, Chatwani A, Harmanli O, Pontari M, Hernandez E. Accuracy of cystoscopy in the diagnosis of ureteral injury in benign gynecologic surgery. Int Urogynecol J Pelvic Floor Dysfunct (2003) 14:427-431.
- Dwyer PL, Carey MP, Rosamilia A. Suture injury to the urinary tract in urethral suspension procedures for stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct (1999) 10:15-21
- Gilmour DT, Dwyer PL , Carey MP. Lower urinary tract injury during gynecologic surgery and its detection by intraoperative cystoscopy. Obstet Gynecol (1999) 94:883-889
- Härkki-Siren P, Kurpi T, Sjöberg J, Tiitinen A. Safety aspects of laparoscopic hysterectomy. Acta Obstet Gynecol Scand (2001) 80:383-391
- Hurd WW, Bude RO, De Lancey JO, Pearl ML. The relationship of the umbilicus to aortic bifurcation: implications for laparoscopic technique. Obstet Gynecol (1992) 80:48-51.
- Kadar N. Dissecting the pelvic retroperitoneum and identifying the ureters. A laparoscopic technique. J Reprod Med (1995) 40:116-122.
- Leonard F, Chopin N, Borghese B, Fotso A, Foulot H, Coste J, Mignon A, Chapron C. Total laparoscopic hysterectomy: preoperative risk factors for conversion to laparotomy. J Minim Invasive Gynecol (2005) 12:312-317.
- O'Shea RT, Petrucco O, Gordon S, Seman E. Adelaide laparoscopic hysterectomy audit (1991-1998): realistic complications rates. Gynaecol Endoscopy (2000) 9:369-372
- Reich H, De Caprio J, McGlynn F. Laparoscopic hysterectomy. J Gynecol Surg (1989) 5:213-216.
- Vakili B, Chesson RR, Kyle BL, Shobeiri SA, Echols KT, Gist R, Zheng YT, Nolan TE. The incidence of urinary tract injury during hysterectomy: a prospective analysis based on universal cystoscopy. Am J Obstet Gynecol (2005) 192:1599-1604.
- Mattingly RF, Thompson JD. In: "Telinde's Operative Gynecology". Ed 6 th . Philadelphia : JB Lippincott Co; 1985.
- Park RC, Duff WP. Role of caesarcan hysterectomy in modern obstetric practice. Clinics in Obstet Gynawcol 1980; 23: 601-620.
- Thompson RH. Ureteral injuries in pelvic surgery. Bull Dept Gyecol Obstet Emory U 1980; 11:93.
- Rodriguez-Armas O, Daya S. Definitions and factors affecting infertility. In: Rodriguez-Armas O, Hedon B, Daya S: Infertility and contraception. Parthenon publishing group, 1998; 1 - 21.
- Bhatthcharya S. Infertility. In: Dewhurst's Textbook of Obstetrics and Gynaecology for Postgraduates. 7th edition. Edmonds DK (ed). Blackwell Publishing 2007; 440-460.
- Drew, G. Assisted Reproduction. In: Dewhurst's Textbook of Obstetrics and Gynaecology. 7th Edition. Edmonds D. K.(ed) Blackwell Publishing 2007; 461-468.
- Ajayi RA. Advances in Assisted Reproduction. Archives of Ibadan Medicine. Olapade-Olaopa,OE(ed). 2(2), 9-12.
- Maghissi, K. S. Introduction to Reproductive Endocrinology. In: Precis. An Update in Obstetrics and Gynecology. ACOG Publication (ix).
- John CT. Coping with the infertile couple. Proceedings of the Second Regional Conference of the Medical Women's International Association Abuja, Benin City. Ambik Press, 2000:159-151.
- Anibue PN, Aniebue UU. Adoption Practices In Enugu , Nigeria . Nigeria Journal of Clinical Practice March 2008; 11(1):5-8.
- Papageorghiou AT. Ethical considerations in embyo-reductio. Current Obstetrics and Gynaecology. 2006; 16, 181-184.
- McMahon C, Gibson F, Leslie G, Tennant C and Saunders D Mothers conceiving through in vitro fertilization: siblings, setbacks and embryo dilemma after five years. Reprod Technol 2000;10, 131-135.
- Laruelle C, Englert Y. Psychological study of in vitro fertilization-embryo transfer participants' attitudes towards the destiny of their supernumerary embryos. Fert. Steril 1995; 63, 1047-1050.
- Lornage J, Chorier H, Bouilieu D, Mathieu C, Czaba JC. Six years' follow-up of cryopreserved human embryos. Human Reprod. 2003; 18,871-877.
- Newton CR, McDermid A, Tekpetey F, Tummon IS. Embryo donation: Attitudes towards donation procedures and factors predicting willingness to donate. Human Reprod 2003; 18, 878-844
- Meldrum DR . In Vitro Fertilization and Embryo Transfer. In: Gynecology and Obstetrics Looseleaf. lippincott Williams & Wilkins 2001; (5) 97
- Orhue A, Aziken M. Experience with a comprehensive university hospital-based infertility program in Nigeria . Intl J Obs. Gynaecol. 2008; 101, 11-15
- Carley ME, Mclntire D, Carley JM,Schaffer J. Incidence, risk factors and morbidity of unintended bladder or bladder or ureter injury during hysterectomy, Int Urogynecol J Pelvic Floor Dysfunct 2002;13:18-21.
- Chapron C, Fauconnier A, Goffinet F, Breart G, Dubuisson JB. Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynecologic pathology. Results of a meta-analysis. Hum Reprod 2002;17:1334-1342
- Dandolu V, Mathai E, Chatwani A, Harmanli O, Pontari M, Hernandez E. Accuracy of cystoscopy in the diagnosis of ureteral injury in denign gynecologic surgery. Int Urgynecol J Pelvic Floor Dysfunct 2003;14:427-431.
- Gilmour DT, Das S, Flowerdew G. Rates of urinary tract injury from gynecologic surgery and the role of intraopearative cystoscopy. Obstet Gynecol 2006; 107:1366-1372.
- Harkki-Siren P, Sjoberg J. Tiitinen A. Urinary tract injury after hysterectomy, Onstet Gynecol 1992;80:48-51.
- Kreiker G, Beroldi A, Sad Larcher J, Ruiz Orrico G, Chapron C. Prospective evaluation of the learning curve of total laparoscopic hysterectomy in a universitary hospital. J Am Assoc Gynecol Laparosc 2004; 11:229-235.
- Meikle SF, Nugent EW, Orleans M. Complications and recovery from laparoscopy-assisted vaginal hysterectomy compared with abdominal and vaginal hysterectomy. Obstet Gynecol 1997; 89:304-311.
- Saidi MH, Sadler RK, Vancaillie TG, Akright BD, Farhart SA, white AJ. Diagnosis and management of serious urinary complicatiosn after major operative laparoscopy Obstet Gynecol 1996; 87:272-276.
- Shen CC, Wu MP, Kung Ft, Huang FJ, Hsieh CH, Lan KC, Huang Ey, Hsu Ty, Chang SY. Major Complications associated with laparoscopic-assisted vaginal hysterectomy: ten-year experience. J Am Assoc Gynecol Laparosc 2003; 10:147-153.
- Baadsgaard, S.E., Bille, S. and Egeblad, K. (1989) Major vascular injury during gynecologic laparoscopy. Acta Obstet. Gynecol. Scand. , 68, 283-285.
- Bateman, B.G., Kolp, L.A. and Hoeger, K. (1996) Complications of laparoscopy: operative and diagnostic. Fertil. Steril. , 66, 30-35.
- Borgatta, L., Gruss, L., Barad, D. et al. (1990) Direct trocar insertion versus veress needle use for laparoscopic sterilization. J. Reprod. Med. , 35, 891-894.
- Byron, J., Markenson, G. and Miyazawa, K. (1993) A randomized comparison of veress needle and direct trocar insertion for laparoscopy. Surg. Gynecol. Obstet. , 177, 259-262.
- Chamberlain, G. and Brown, J.D. (1978) Gynecologic laparoscopy. Report of the working party of the confidential enquiry into gynaecological laparoscopy. Br. J. Obstet. Gynaecol. , 85, 401-403.
- Chapron, C. and Querleu, D. (1994) Complications de l'Endoscopie Ope´ratoire en Gyne´cologie. Arnette, Paris , France .
- Chapron, C., Devroey, P., Dubuisson, J.B. et al. (1997a) ESHRE guidelines for training, accreditation and monitoring in gynaecological endoscopy. Hum. Reprod. , 12, 867-868.
- Chapron, C., Pierre, F., Lacroix, S. et al. (1997b) Major vascular injuries during gynecologic laparoscopy. J. Am. Coll. Surg. , 185, 461-465.
- Gomel , V. and James, S. (1991) Intraoperative management of ureteric injury during operative laparoscopy. Fertil. Steril. , 55, 416-419.
- Harkki-Siren, P. and Kurki, T. (1997) A nationwide analysis of laparoscopic complications. Obstet. Gynecol. , 89, 108-112.
- Hasson, H.M. (1971) A modified instrument and method for laparoscopy. Am. J. Obstet. Gynecol. , 110, 886-887.
- Hulka, J.F., Peterson, H.B., Surrey , M. et al. (1987) American Association of Gynecologic Laparoscopists' 1985 membership survey. J. Reprod. Med. , 32, 732-735.





