Dr. Azza Gouda Attia, M.B.B.Ch; Arab board specialization; MRCOG; D.MAS;
Senior specialist Obstetrician and Gynecologist
Al wasl Hospital, Dubai, UAE.
Member of World Association of Laparoscopic Surgeons
Senior Consultant Laparoscopic Surgeon
Director, World Laparoscopy Hospital, Gurugram, NCR Delhi
Member World Association of Laparoscopic Surgeon
Member Indian Association of Gastrointestinal Endosurgeons
Member Society of American Gastrointestinal and Endoscopic Surgeons
Project submitted towards completion of Diploma in Minimal Access Surgery, World Laparoscopy Hospital, Gurugram, NCR Delhi, INDIA. MAY 2007
Abstract
Tubal prolapse is an uncommon but frequently reported complication of hysterectomy. This article is review of studies and case reports comparing laparoscopic versus open management of tubal prolapse. This review compares 20 studies and case reports available from many countries. The consensus favored that tubal prolapse can be diagnosed and successfully managed with laparoscopic approach.
Keywords
Tubal prolapse, Fallopian tube prolapse, Management of tubal prolapse, Laparoscopic role in the management of tubal prolapse.
Introduction
Fallopian tube prolapse into the vaginal vault is a rare complication after hysterectomy with adnexal conservation. The initial case was reported by Pozzi in 1902 since that sporadic cases of tubal prolapse and different methods of management have been added to the literature.
Treatment modalities have been described by vaginal, abdominal and combined approach .Laparoscopic management more recently advocated in combination with vaginal approach with partial or complete Salpingectomy. Tubal prolapse maybe considered as hernia and occurs if a communication exists between the peritoneal cavity and vaginal canal.1
The exact incidences of fallopian tube prolapse is difficult to estimate because cases may go undiagnosed and may resolve before detection.
As has been noted by others, prolapse of fallopian tube following vaginal or abdominal hysterectomy is probably much more common than the number of reports the literature indicates 26,27 .
Fallopian tube prolapse after the vaginal hysterectomy is more common than after abdominal hysterectomy 1,23. however it was also reported that most of the cases occurred after abdominal hysterectomy2.
Symptoms
The patient may present two months to 30 years after surgery with profuse vaginal discharge, leucorrhea, persistent blood loss, dysparenia and chronic pelvic pain. Patient maybe asymptomatic 2 And observation alone may lead to resolution. Apart from vagina, urinary bladder and uterus are the other two infrequent sites of prolapsed tube 3,4
Predisposing factors
Tubal prolapse can occur following abdominal, vaginal hysterectomy, rarely following laparoscopic hysterectomy and colpotomy. Inadequate preparation of the vagina ,Vaginal infection, febrile episodes ; post operative bleeding, hematoma formation, failure to close securely the tissues at the vaginal vault, presence of vaginal drainage in cul-de-sac ,defective surgical technique, operative difficulty, lake of accurate hemostasis and poor physical condition of the patient are the most important predisposing factors for intravaginal tubal prolapse 5,6
Diagnosis
The diagnosis is often delayed and has usually not been made prior to biopsy (except in rare cases where fimbrial end had prolapsed) as the clinical appearance is that of granulation tissue, so it is necessary to receive pathological confirmation by performing vaginal biopsy when fallopian tube prolapse is clinically suspected 6,7. The diagnosis of fallopian tube prolapse should be suspected when a red granular, polypoid mass or lesion is seen at the vaginal cuff protruding into the vagina after hysterectomy.
Differential Diagnosis
Symmonds et al 8 have pointed that the fallopian tube tissue is firmer than usual granulation tissue and is also more tender. The easy passage of a probe into the lumen of the tube or the abdominal cavity will help in establishing the diagnosis.
The presence of vaginal tubal epithelial cells in the vaginal smear after hysterectomy is also a point in favor of tubal prolapse 9
Varnoholt H et al 10 have pointed out that fallopian tube prolapse may show an unusual resemblance of aggressive angiomyxoma and thus poses a diagnostic pitfall
Wheelock J B et al 11 stated that vaginal prolapse of fallopian tube in postmenopausal patients presented with an erroneous diagnosis of adenocarcinoma of vaginal apex. Failure to consider fallopian tube prolapse in the differential diagnosis of vaginal adenocarcinoma may lead to unnecessary intervention with subsequent complications.
Jashnai K D et al 6 have pointed out that squamous metaplasia may occur due to chronic irritation and severe inflammation. If squamous metaplasia is extensive it can conceal the normal tubal epithelium and make the diagnosis difficult. Also, it may lead to malignant transformation.
T Lefrancq et al 12 described unusual association of fallopian tubal prolapse and herpetic infection. He stated that direct exposure of the herniated fallopian tube to various pathogens in the vagina provides an unique clinical model for salpingitis.In herpetic tubal infection special attention must be paid to cytological atypia to avoid a misdiagnosis of malignancy.
The probability of prolapsed fallopian tube should be remembered in the differential diagnosis in all cases of vaginal lesions found after hysterectomy particularly when the operation has been performed by vaginal route.
Materials and Methods
A literature search was performed using Medline and search engine Google to find related articles. The following search words were used: Tubal prolapse, fallopian tube prolapse, management of tubal prolapse, laparoscopic role in the management of tubal prolapse
management of Tubal Prolapse
Keith W. K Lo et al 13 presented his experience in the management of seven cases of fallopian tube prolapse with different surgical approaches according to the characteristic of the case .It is suggested that the choice between abdominal ; vaginal and combined laparoscopic approach with partial or complete salpingectomy in the management of prolapsed tube must be individualized according to the patients characteristics and presenting symptoms .Laparoscopic surgery has a role in cases with intraperitoneal adhesions as it safely allow mobilization of the prolapsed tube with complete removal and resolution of symptoms.
Three cases of his series who presented with post - coital bleeding were treated with vaginal partial salpingectomy. One case who complained of pelvic pain and dysparenia required a vaginal total salpingectomy to remove the upper intraperitoneal portion of the tube that caused the pain. Two cases that were expected to have dense adhesions were managed with total salpingectomy using combined vaginal and laparoscopic approach.
Gerard S. Letterie et al 14 managed two cases of tubal prolapse by a combined vaginal and laparoscopic approach, total salpingectomy was done with minimal difficulty and limited invasiveness. The combined technique allows adhesiolysis, full mobilization of the involved adnexal and total salpingectomy with limited dissection.
>Total Salpingectomy has been recommended as optimal management 14 because recurrent symptoms have been reported after partial salpingectomy.However; severe pelvic adhesions prevent adequate laparoscopic visualization and mobilization of the tube an abdominal approach although more invasive should be used.
David M. Rosenthal et al 15 reported a case of fallopian tube prolapse after laparoscopic resection of pelvic endometriosis .He stated that laparoscopic surgery when associated with creation of a vaginal peritoneal fistula is a risk factor for tubal prolapse.Careful closure of vaginal defect during operative laparoscopy and slow release of pneumoperitoneum under direct vision is essential to prevent this complication. This problem can be diagnosed and safely managed with laparoscopic approach with excellent chance of cure.
Rivlin, Michel E et al 16 report a total laparoscopic technique for initial management of fallopian tube prolapse .Patient was presented one year after vaginal hysterectomy; an outpatient laparoscopic salpingo-oophorectomy was performed with laparoscopic closure of vaginal defect. He suggests that laparoscopic surgery can be used successfully without the need for a combined vaginal approach.
The aim of different surgical approaches is to remove the inflammatory tube from the vaginal vault, to close the vagino-peritoneal defect and to relieve the symptoms. The different approaches include vaginal route, combined vaginal and laparoscopic route or even abdominal route.16
Wetchler el al 17 published their technique in vaginal total salpingectomy .It is done by making an elliptical incision in the vaginal cup around the prolapsed tube followed by dividing peritubular adhesion under direct vision which allows complete resection of the tube .Total excision by vaginal approach is sometimes difficult due to dense bowel,bladder,or adnexal adhesions that prevent full mobilization of the involved tube. Batty and Colleagues 18 first used laparoscopy to aid in the excision of prolapsed vaginal tube.
Procedure
During the procedure of combined vaginal and laparoscopic approach the standard method of insufflations of the abdominal cavity is via a Veress needle inserted through a small skin incision in the infra umbilical region.
Initially at the time of pneumoperitoneum by veress needle, patient should be placed supine with 10-20 degrees head down. The benefit of this steep trendelenburg position is that bowel will be pulled up and there will be more room in pelvic cavity for safe entry of veress needle. It is important to remember that patient should be placed in head down position only if surgeon is planning to insert veress needle pointing towards pelvis cavity. If surgeon is planning to insert veress needle perpendicular to abdominal wall as in case of very obese patient. The patient should be placed in supine position otherwise all the bowel will come just below the umbilicus and there is increased risk of bowel injury.
Patient should be positioned in lithotomy position and one assistant should be positioned between the leg of patient. Patient's leg should be comfortably supported by padded obstetric leg holders or Allen stirrups which minimizes the risk of venous thrombosis. In these procedure surgeon need to use uterine manipulator for proper visualization of female reproductive organs.
As soon as 100 to 200 ml of gas is inside the abdominal cavity surgeon should do percussion of the right hypochondria and liver dullness should obliterate with tympanic sound. Normal size human abdominal cavity need 1.5 liter CO2 to achieve intra-abdominal actual pressure of 12 mm Hg. In some big size abdominal cavity and in multipara patients sometime we need 3 liter of CO2 (rarely 5 to 6 liters) to get desired pressure of 12mm Hg.
In same manner all the working port should be introduced and instruments are inserted to start the surgery. It should be remembered that distance between two ports should never be less than 5cm. The "Baseball Diamond Concept" is the most appropriate method to decide the site of introduction of working port The positioning of operative ports is an important factor in determining the ease with which a procedure is carried out.
After laparoscopic visualization of the pelvis and adnexal structures 14 ,an elliptical incision done around the prolapsed tube in the vaginal mucosa .The tube freed from mucosal and peritoneal attachment by sharp dissection (Fig-1). Two Allis clamps were then placed at the vaginal incision permitting establishment of a pneumoperitoneum (Fig-2). Standard laparoscopic technique was used with additional ports in the suprapubic region and at Mc Burney's point .These sites were used for insertion of bipolar forceps, grasping forceps and laparoscopic scissors. Pelvic adhesion were incised, freeing the tube from pelvic sidewall ,bowel attachment and mobilizing it on the mesosalpinx.while maintaining traction on the tube with grasping forceps total salpingectomy was accomplished using bipolar and scissor to alternatively coagulate and incise the mesosalpinx (Fig-3). When free from all attachments tube was withdrawn through 10 mm trocar inserted through the suprapubic port. The pelvic peritoneum and vaginal mucosa were closed. Following surgery complete symptom resolution is usually observed and no recurrence has been report.
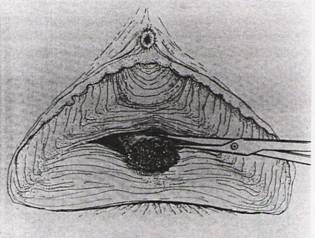
Figure-1 Prolapsed tube sharply dissected from vaginal mucosa pelvic peritoneum using Metzenbaum scissors.

Figure-2 Vaginal mucosa temporarily re approximated at vaginal incision using two Ellis clamps.

Figure-3 Total Salpingectomy accomplished laparoscopicallyby dividing the mesosalpinx using Kleppinger bipolar forceps grasping forceps, and laparoscopic scissors.
Discussion
Though rare; fallopian tube prolapse may cause symptoms serious enough to warrant treatment. Total salpingectomy was recommended as optimal management because recurrent symptoms have been reported after partial salpingectomy.
If vaginal approach is difficult due to dense bowel, bladder, and or adnexal adhesion that prevent full mobilization of the prolapsed tube, partial salpingectomy or abdominal approach must be considered.
The combined technique of simultaneous laparoscopic and limited vaginal approach for management of fallopian tube prolapse allow adhesiolysis,Full mobilization of the involved tube and total salpingectomy with minimal dissection and invasivness.This method should be applicable in most clinical conditions when salpingectomy is indicated and cannot done vaginally .It can be done on outpatient basis thus limiting hospitalization.
When severe pelvic adhesions prevent adequate laparoscopic visualization and mobilization of the tube, an abdominal approach although more invasive should be used.
There is growing trend toward laparoscopic approach because it decrease wound morbidity, reduce length of hospital stay with quicker recovery.
Hence, the procedure can be completed entirely laparoscopically in the presence of appropriate surgical training with vault closure using extracorporeal or intracorporeal technique.
Vaginal removal of the prolapsed tube with laparoscopic surgery may be suitable treatment. The abdominal or vaginal approach used in surgical management of prolapsed tubes must be decided according to the patient individual characteristics.
Conclusion
Surgical excision remain the treatment of choice for symptomatic fallopian tube prolapse. It is inadequate to try local destruction or application of caustic agents as reoccurrences and pain are the most likely sequels. This is probably due to the continues traction on the remaining portion of the prolapse fallopian tubes. Therefore women with either pelvic pain or pain during coitus as a major symptoms should be treated with total salpimgectomy.
After going through all the literature it was found that combined laparoscopic and vaginal approach management of tubal prolapse should be applicable in most clinical circumstances when salpimgectomy is indicated as it provides the advantages of total salpimgectomy without laparotomy and may performed as a day case and it should be accepted by repertoire of practicing gynecologists.
REFERENCES
[1] Candiani G B ,Candian M; Posthysterectomy Fallopian Tube hernia .a report of two cases. J Reprod Med.1996 Dec;41{12 ; 915-20
[2] RaminSm ,Ramin KD ,Hemsell DL ,Fallopian tube prolapse after hysterectomy, South Med;1999 Oct,92{10} ;963-6
[3] Anastasiades KD; Majmudar B.Prolapse of Fallopian tube into urinary bladder, mimicking bladder carcinoma. Arch Pathol Lab Med 1983; 107; 613-4
[4] Stiegad S J , Margin C T Fallopian tube presenting as uterine polyp. Aust NZ /Obstet Gynaecol 1978; 18; 281-3.
[5] Mustafa Kucuk , Laparoscopic management of fallopian tube prolapse masquerading as adenocarcinoma of the vagina .in hysterectomized woman, BMC women's Health 200,2;2
[6] Jashnani KD, Naik LP;Prolapsed Fallopian tube with squamous metaplasia ,J Postgrad Med 2002 ;48 ;241-2
[7] Song YS,Kang JS ,Park MH;Fallopian tube prolapse misdiagnosed as vault granulation tissue .a report of three cases ,san gdong -KU;133-791 Seoul; Korea .
[8] Symmonds RE;Counceller VS; Prattjh .Prolapse of a fallopian tube as complication of hysterectomy .AmjObstet Gynecol 1957;74;214-7 .
[9] Hellen EA ,Cghill SB,Clark JV .Prolapsed Fallopian tube after abdominal hysterectomy ,a report of the cytological findings cytopathology 1993;4;181-5
[10] Varanholth Otis Cn ,Nucci MR;Johari VP ,Fallopian tube prolapse mimicking aggressive angiomyxoma J Gynecol pathol,2005 Jul ;24[3];292-4 .
[11] WHEELOCK JB,Schniderv Goplerud DR, prolapsed fallopian tube masquerading as adnocarcinoma of the vagina in a postmenopausal women.Gynecol on col,1985 July;{3] ;369-75 .
[12] Lefrancq, T; Orain, I; Michalak, S; Hourseau, M; Fetissof, F Herpetic salpingitis and fallopian tube prolapse Histopathology, Volume 34, Number 6, June 1999, pp. 548-550(3)
[13] Keith WH.LO,The role of laparoscopic surgery in the management of tubal prolapse ,A 7 case series and literature Review .surgical innovation volume 14 number 1march 2007 24-26 .
[14] Gerard S .Letterie, laparoscopic management of fallopian tube prolapse. Obstet Gynecol; 72; 508; 1988.
[15] David M .Rosenthal, fallopian tube prolapse after laparoscopic resection of pelvic endometriosis, Obstet Gyncol 2005; 105; 8.8-9 .
[16] Rivlin; Michel E, Total laparoscopic management of fallopian tube prolapse, case report; Journal of pelvic medicine and surgery .12{1]; 53-55; January / February 2006 .
[17] Wetchler SJ, Hurt WG .Atechnique for surgical correction of fallopian tube prolapse .Obstet Gynecol .1986; 76; 747-749.
[18] Batty LH Williams,SB,Krantz KE laparoscopy repair of the prolapsed fallopian tube .J Reprod Med.1980 ;24;244-246 .
[19] C R Hernandeez , management of tubal prolapse after hysterectomy .Jam Assoc Gynecol laprosc,Feb,1998;5[1];59-62 .
[20] Jensen H, Prolapse of the salpinx after hysterectomy, Ugeskrlaeger, 1996 Sep 2; 158; [36]; 5040-1
[21] Iavy Y ,Hamani ,levsagie A ,Fallopian tube prolapse after hysterectomy ,Hare Fuah .2002 Jun ;141 [6] ;530-1,578 .
[22] Lenglet ,Pyosalpingitis after intradenxal laparoscopic hysterectomy, two cases ,Obstet Fertil,2005 Oct;33 [10] ;768-71 .
[23] Muntz HG, Fallopian tube prolapse after hysterectomy, A report of 2 cases, JReprod Med .1988;33 [5];467-9 .
[24] Noor S, Fallopian tube prolapse after abdominal hysterectomy .JAyub Med Coll Abbtta bad.2004 April -Jun; 16[2]; 78-9.
[25] Byrne DL, Edmonds DK.Prolapse of fallopian tube following abdominal hysterectomy.JR Sos Med .1989; 82; 746; 765.
[26] Carmicahael DG; Prolapsed of fallopian tubes in to the vaginal vault. Am J Obstet GyneCol 1976, 125:266-267.
[27] De Clippelle, Coenen M, Bhal PS, Amson: fallopian tubes prolapse following abdominal hysterectomy. Aust NZJ Obstet GyneCol 2001,41:106-108.





