Page 52 - World Journal of Laparoscopic Surgeons
P. 52
Malwinder Singh et al
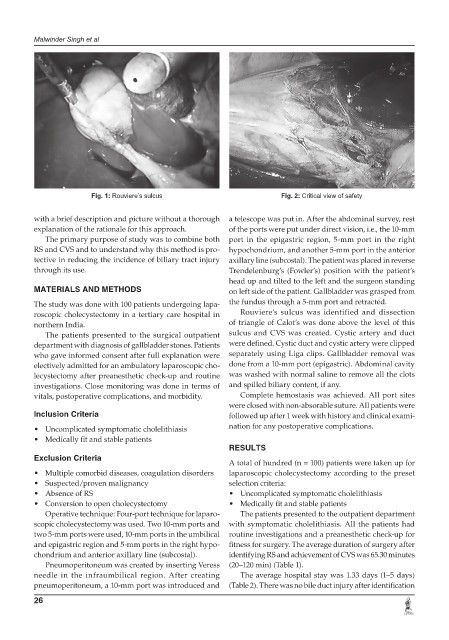
Fig. 1: Rouviere’s sulcus Fig. 2: Critical view of safety
with a brief description and picture without a thorough a telescope was put in. After the abdominal survey, rest
explanation of the rationale for this approach. of the ports were put under direct vision, i.e., the 10-mm
The primary purpose of study was to combine both port in the epigastric region, 5-mm port in the right
RS and CVS and to understand why this method is pro- hypochondrium, and another 5-mm port in the anterior
tective in reducing the incidence of biliary tract injury axillary line (subcostal). The patient was placed in reverse
through its use. Trendelenburg’s (Fowler’s) position with the patient’s
head up and tilted to the left and the surgeon standing
MATeRIALS AND MeTHODS on left side of the patient. Gallbladder was grasped from
The study was done with 100 patients undergoing lapa- the fundus through a 5-mm port and retracted.
roscopic cholecystectomy in a tertiary care hospital in Rouviere’s sulcus was identified and dissection
northern India. of triangle of Calot’s was done above the level of this
The patients presented to the surgical outpatient sulcus and CVS was created. Cystic artery and duct
department with diagnosis of gallbladder stones. Patients were defined. Cystic duct and cystic artery were clipped
who gave informed consent after full explanation were separately using Liga clips. Gallbladder removal was
electively admitted for an ambulatory laparoscopic cho- done from a 10-mm port (epigastric). Abdominal cavity
lecystectomy after preanesthetic check-up and routine was washed with normal saline to remove all the clots
investigations. Close monitoring was done in terms of and spilled biliary content, if any.
vitals, postoperative complications, and morbidity. Complete hemostasis was achieved. All port sites
were closed with non-absorable suture. All patients were
Inclusion Criteria followed up after 1 week with history and clinical exami-
• Uncomplicated symptomatic cholelithiasis nation for any postoperative complications.
• Medically fit and stable patients
ReSULTS
exclusion Criteria
A total of hundred (n = 100) patients were taken up for
• Multiple comorbid diseases, coagulation disorders laparoscopic cholecystectomy according to the preset
• Suspected/proven malignancy selection criteria:
• Absence of RS • Uncomplicated symptomatic cholelithiasis
• Conversion to open cholecystectomy • Medically fit and stable patients
Operative technique: Four-port technique for laparo- The patients presented to the outpatient department
scopic cholecystectomy was used. Two 10-mm ports and with symptomatic cholelithiasis. All the patients had
two 5-mm ports were used, 10-mm ports in the umbilical routine investigations and a preanesthetic check-up for
and epigastric region and 5-mm ports in the right hypo- fitness for surgery. The average duration of surgery after
chondrium and anterior axillary line (subcostal). identifying RS and achievement of CVS was 65.30 minutes
Pneumoperitoneum was created by inserting Veress (20–120 min) (Table 1).
needle in the infraumbilical region. After creating The average hospital stay was 1.33 days (1–5 days)
pneumoperitoneum, a 10-mm port was introduced and (Table 2). There was no bile duct injury after identification
26