Page 54 - Journal of World Association of Laparoscopic Surgeons
P. 54
Minimal Invasive Management of Gallbladder Perforation
There are several mechanisms behind GBP. The most common in a number of sign and symptoms including generalized or right
is cystic duct obstruction, gallbladder distension, altered upper quadrant pain, fever, and jaundice.
vascularization, ischemia, and necrosis followed by perforation. Patients can also present with generalized peritonitis and
Fundus of the gallbladder is the most common site of septic shock.
perforation secondary to its poor blood supply. GBP can represent Gore et al. suggested that GBP should be suspected in patients
of acute cholecystitis who suddenly deteriorated and become
Table 1: Neimeier classification of gallbladder perforation toxic. 8
Ultrasonography is the initial radiological investigation done in
Type State Description most of the cases, but it has its own limitations in suspected cases
Type I Acute Is associated with generalized biliary of GBP due to gaseous distension of bowel and pain; sonography
peritonitis is compromised and unable to locate the perforation. CT scan is
Type II Subacute Consists of fluid localization at perforation considered the gold standard for the diagnosis of complicated biliary
site, pericholecystic abscess pathology. Signs of GBP on CT scan include a defect, thickening,
10
Type III Chronic Includes the formation of internal or external and enhancement in gallbladder wall and gall stones in common bile
fistulas duct and cystic duct. Pericholecystic changes include fat stranding,
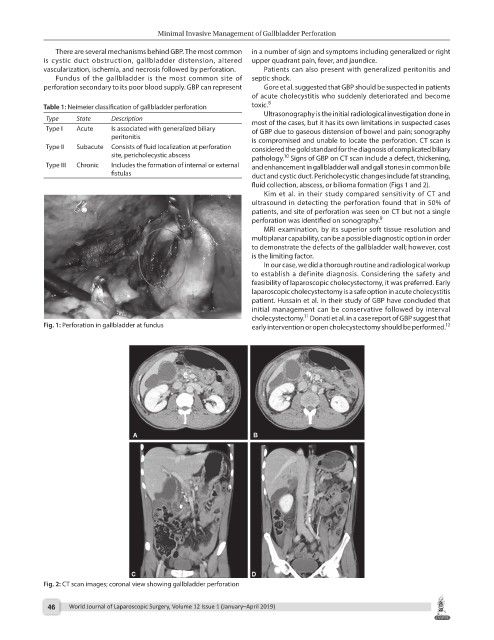
fluid collection, abscess, or bilioma formation (Figs 1 and 2).
Kim et al. in their study compared sensitivity of CT and
ultrasound in detecting the perforation found that in 50% of
patients, and site of perforation was seen on CT but not a single
perforation was identified on sonography. 9
MRI examination, by its superior soft tissue resolution and
multiplanar capability, can be a possible diagnostic option in order
to demonstrate the defects of the gallbladder wall; however, cost
is the limiting factor.
In our case, we did a thorough routine and radiological workup
to establish a definite diagnosis. Considering the safety and
feasibility of laparoscopic cholecystectomy, it was preferred. Early
laparoscopic cholecystectomy is a safe option in acute cholecystitis
patient. Hussain et al. in their study of GBP have concluded that
initial management can be conservative followed by interval
11
cholecystectomy. Donati et al. in a case report of GBP suggest that
Fig. 1: Perforation in gallbladder at fundus early intervention or open cholecystectomy should be performed. 12
Fig. 2: CT scan images; coronal view showing gallbladder perforation
46 World Journal of Laparoscopic Surgery, Volume 12 Issue 1 (January–April 2019)