Page 46 - World Journal of Laparoscopic Surgery
P. 46
Dysphagia after Bougie-guided Crural Repair
resolved within 8 weeks postoperatively, while late dysphagia
was defined by having PD that time and requires endoscopic
intervention and/or surgery for resolution. 13,14
Any investigations required for postoperative dysphagia were
recorded.
results
All our 40 patients had laparoscopic Nissen fundoplication using
our technique for chronic GERD with sliding hiatal hernia during
the given period of time.
The study included 10 males (25%) and 30 females (75%). The
median age was 44 years. Sliding hiatal hernias were detected
in all patients as proven by preoperative upper GI endoscopy
with sizes ranging from 1 to 5 cm. Four patients (10%) showed
Barrett’s metaplasia with no dysplasia in the histology taken upon
esophagogastroduodenoscopy (EGD) before the procedure. All
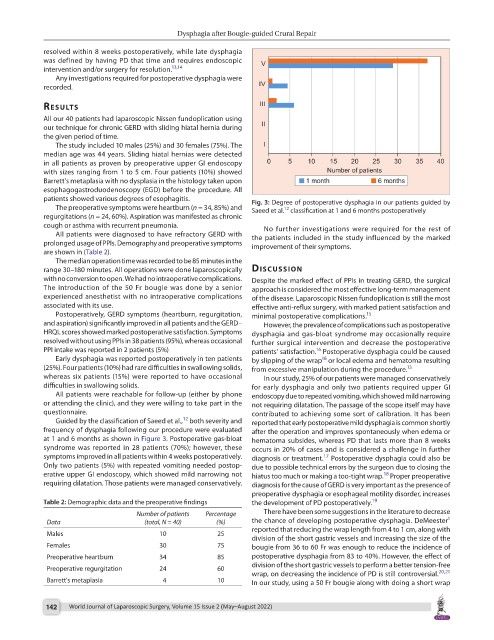
patients showed various degrees of esophagitis. Fig. 3: Degree of postoperative dysphagia in our patients guided by
The preoperative symptoms were heartburn (n = 34, 85%) and Saeed et al. classification at 1 and 6 months postoperatively
12
regurgitations (n = 24, 60%). Aspiration was manifested as chronic
cough or asthma with recurrent pneumonia. No further investigations were required for the rest of
All patients were diagnosed to have refractory GERD with the patients included in the study influenced by the marked
prolonged usage of PPIs. Demography and preoperative symptoms improvement of their symptoms.
are shown in (Table 2).
The median operation time was recorded to be 85 minutes in the
range 30–180 minutes. All operations were done laparoscopically dIscussIon
with no conversion to open. We had no intraoperative complications. Despite the marked effect of PPIs in treating GERD, the surgical
The introduction of the 50 Fr bougie was done by a senior approach is considered the most effective long-term management
experienced anesthetist with no intraoperative complications of the disease. Laparoscopic Nissen fundoplication is still the most
associated with its use. effective anti-reflux surgery, with marked patient satisfaction and
Postoperatively, GERD symptoms (heartburn, regurgitation, minimal postoperative complications. 15
and aspiration) significantly improved in all patients and the GERD– However, the prevalence of complications such as postoperative
HRQL scores showed marked postoperative satisfaction. Symptoms dysphagia and gas-bloat syndrome may occasionally require
resolved without using PPIs in 38 patients (95%), whereas occasional further surgical intervention and decrease the postoperative
PPI intake was reported in 2 patients (5%) patients’ satisfaction. Postoperative dysphagia could be caused
16
Early dysphagia was reported postoperatively in ten patients by slipping of the wrap or local edema and hematoma resulting
16
(25%). Four patients (10%) had rare difficulties in swallowing solids, from excessive manipulation during the procedure.
13
whereas six patients (15%) were reported to have occasional In our study, 25% of our patients were managed conservatively
difficulties in swallowing solids. for early dysphagia and only two patients required upper GI
All patients were reachable for follow-up (either by phone endoscopy due to repeated vomiting, which showed mild narrowing
or attending the clinic), and they were willing to take part in the not requiring dilatation. The passage of the scope itself may have
questionnaire. contributed to achieving some sort of calibration. It has been
12
Guided by the classification of Saeed et al., both severity and reported that early postoperative mild dysphagia is common shortly
frequency of dysphagia following our procedure were evaluated after the operation and improves spontaneously when edema or
at 1 and 6 months as shown in Figure 3. Postoperative gas-bloat hematoma subsides, whereas PD that lasts more than 8 weeks
syndrome was reported in 28 patients (70%); however, these occurs in 20% of cases and is considered a challenge in further
symptoms improved in all patients within 4 weeks postoperatively. diagnosis or treatment. Postoperative dysphagia could also be
17
Only two patients (5%) with repeated vomiting needed postop- due to possible technical errors by the surgeon due to closing the
erative upper GI endoscopy, which showed mild narrowing not hiatus too much or making a too-tight wrap. Proper preoperative
18
requiring dilatation. Those patients were managed conservatively. diagnosis for the cause of GERD is very important as the presence of
preoperative dysphagia or esophageal motility disorder, increases
Table 2: Demographic data and the preoperative findings the development of PD postoperatively. 19
Number of patients Percentage There have been some suggestions in the literature to decrease
1
Data (total, N = 40) (%) the chance of developing postoperative dysphagia. DeMeester
reported that reducing the wrap length from 4 to 1 cm, along with
Males 10 25
division of the short gastric vessels and increasing the size of the
Females 30 75 bougie from 36 to 60 Fr was enough to reduce the incidence of
Preoperative heartburn 34 85 postoperative dysphagia from 83 to 40%. However, the effect of
division of the short gastric vessels to perform a better tension-free
Preoperative regurgitation 24 60
wrap, on decreasing the incidence of PD is still controversial. 20,21
Barrett's metaplasia 4 10 In our study, using a 50 Fr bougie along with doing a short wrap
142 World Journal of Laparoscopic Surgery, Volume 15 Issue 2 (May–August 2022)