Page 68 - World Journal of Laparoscopic Surgery
P. 68
Medtronic I-Drive vs Ethicon Echelon
Methods complication, mortality rate, and stapler cost (government and
We designed a randomized control trial that received institutional commercial rate). The reload time for each staple load was defined
as the time from when the stapler exited the trocar until the stapler
IRB approval. All patients underwent surgery at our facility after was ready to be fired again, which we defined as when the stapler
completing our institutional bariatric pathway to include bariatric was handed back to the surgeon or placed on the Mayo stand
seminars, support groups, extensive medical workup, and if the surgeon was not ready to staple. A physician who was not
psychological evaluation. We excluded patients from participating participating in the operative portion of the case was present to
in the study if they needed revisional surgery or presented with time the surgery. We recorded stapler misfires and results of leak
inflammatory bowel disease. We counseled all patients that each tests, which were determined by the operative surgeon. A Mann-
of the linear staplers used in the study are approved devices for Whitney test was used to compare the distribution of reload times
their surgery and the surgeons performing the operation trained between the two groups.
to operate with both devices. A total of 63 patients consented to The cost for civilian vs government institutions for staplers,
participate in the study and randomized to each arm. staple loads, and reinforcements was gathered from the
The Ethicon Echelon powered stapler—with and without government supply-ordering website and included in the analysis.
Seamguard—and the Medtronic I-Drive powered stapler The cost of each surgery for the Ethicon Echelon was calculated by
with reinforcement comprised the two arms of the study. All adding the cost of the color of load, the number of Seamguards that
laparoscopic sleeve gastrectomies were performed with an were used, and the cost of the disposable stapler. The Medtronic
absorbable polymer membrane staple line reinforcement. The I-Drive cost was calculated by the cost of the color of load with the
majority of surgeons in this study elected to use Seamguard pre-attached reinforcement. The cost of the I-Drive stapler was
on all Echelon loads except for the load most proximal to not included as it is not disposable. We did not include the cost of
the gastroesophageal junction. There were 7 staff surgeons Seamguards or loads that were opened but not used. We performed
and 19 residents that participated in the study. Patients were a pooled t-test to compare the two groups.
randomized into each arm at the time of their consent to the
study. Two researchers performed the randomization sequence
by annotating the study arm on a sheet of paper along with an results
arbitrary sequential numerical identifier, which were stored in a We consented 63 patients for the study and randomized
secure envelope and blindly drawn at the time of consent. We participants into the Echelon with Seamguard (ESG) or I-Drive
enrolled all patients that consented within the study period, with EndoGIA reinforcement arms (GIA-R) between January
and an interim analysis demonstrated a prohibitive number of 2018 and May 2019—we terminated recruitment due to difficulty
participants would be necessary to demonstrate statistically obtaining additional participants. There were 31 patients in the
significant data—at which point study recruitment was concluded ESG arm and 32 in the GIA-R arm. After fall-out, a total of 51
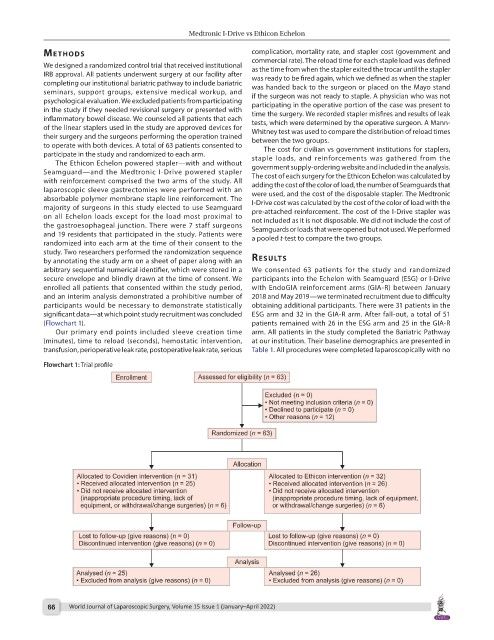
(Flowchart 1). patients remained with 26 in the ESG arm and 25 in the GIA-R
Our primary end points included sleeve creation time arm. All patients in the study completed the Bariatric Pathway
(minutes), time to reload (seconds), hemostatic intervention, at our institution. Their baseline demographics are presented in
transfusion, perioperative leak rate, postoperative leak rate, serious Table 1. All procedures were completed laparoscopically with no
Flowchart 1: Trial profile
66 World Journal of Laparoscopic Surgery, Volume 15 Issue 1 (January–April 2022)