Page 45 - tmp
P. 45
COVID-19 and Surgical Preparedness
412 responses were received, out of which 318 were valid responses and triage for COVID-19 at their workplace. On comparing this
in terms of completeness of proforma. The data so collected were between public and private sectors, the probability of following
compiled and statistically analyzed by SPSS v.21 (IBM). these standard protocols and triage for COVID-19 in practice was
1.68 times higher among private practitioners—132 (79.5%) cases,
results than among those in public healthcare personel—34 (20.4%) cases.
Three-hundred and eighteen responses received were analyzed. The difference was statistically significant (p = 0.02).
One-hundred and forty-three (44.9%) respondents reported
Mean age of the responding surgical specialist was 42.3 ± 10 years. the presence of dedicated COVID-19 recovery wards. This response
Male-to-female ratio of the respondent was 2.38:1 (male = 224, number was significantly higher in private healthcare providers,
female = 94). Most of the respondents, i.e., 168 (52.8%), were aged i.e., 118 (82.5%), than in public healthcare providers, i.e., 25 (17.4%),
between 40 and 59 years (Table 1). Majority of the respondents, p = 0.006.
i.e., 130 (40.8%), were from general surgical specialty (Table 2) Just 34 (10.6%) of the respondents admitted to having
followed by ophthalmology 42 (13.2%), obstetrics and gynecology a negative-pressure operation theater and 15 (4.7%) of the
37 (11.6%), orthopedics 35 (11.0%), and otolaryngology 32 (10.0%). respondents claimed to have separate staff for operating COVID-19
One-hundred and twenty-two out of 224 male respondents were suspected or confirmed cases. However, no statistically significant
general surgeons and 37 out of 94 female respondents were difference was found between public and private care in relation to
practicing in obstetrics and gynecology. the availability of negative-pressure operation theater (p = 0.2) and
The respondents were further categorized into two sectors— dedicated separate auxiliary staff for COVID-19 surgeries (p = 0.07).
private (n = 238) and public health (n = 80)—to assess the Two-hundred and fourteen (67.2%) respondents stated that
level of preparedness for performing surgical procedures and they usually get patients tested for COVID-19 before elective
interventions in the COVID-19 pandemic (Table 3). As far as the surgery (Table 4). This response was largely from the private
health institutional infrastructure and policies were concerned, 166 healthcare providers, i.e., 192 (89.7%), as compared to public
(52.2%) respondents reported the existence of standard protocol
healthcare providers, i.e., 22 (10.2%). The likelihood of presurgery
testing for COVID-19 was 11.04 times higher in private healthcare
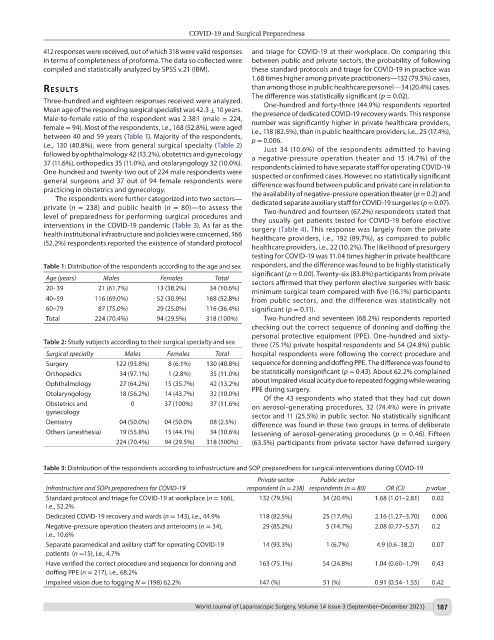
Table 1: Distribution of the respondents according to the age and sex responders, and the difference was found to be highly statistically
significant (p = 0.00). Twenty-six (83.8%) participants from private
Age (years) Males Females Total sectors affirmed that they perform elective surgeries with basic
20–39 21 (61.7%) 13 (38.2%) 34 (10.6%) minimum surgical team compared with five (16.1%) participants
40–59 116 (69.0%) 52 (30.9%) 168 (52.8%) from public sectors, and the difference was statistically not
60–79 87 (75.0%) 29 (25.0%) 116 (36.4%) significant (p = 0.11).
Total 224 (70.4%) 94 (29.5%) 318 (100%) Two-hundred and seventeen (68.2%) respondents reported
checking out the correct sequence of donning and doffing the
personal protective equipment (PPE). One-hundred and sixty-
Table 2: Study subjects according to their surgical specialty and sex three (75.1%) private hospital respondents and 54 (24.8%) public
Surgical specialty Males Females Total hospital respondents were following the correct procedure and
Surgery 122 (93.8%) 8 (6.1%) 130 (40.8%) sequence for donning and doffing PPE. The difference was found to
Orthopedics 34 (97.1%) 1 (2.8%) 35 (11.0%) be statistically nonsignificant (p = 0.43). About 62.2% complained
Ophthalmology 27 (64.2%) 15 (35.7%) 42 (13.2%) about impaired visual acuity due to repeated fogging while wearing
PPE during surgery.
Otolaryngology 18 (56.2%) 14 (43.7%) 32 (10.0%) Of the 43 respondents who stated that they had cut down
Obstetrics and 0 37 (100%) 37 (11.6%) on aerosol-generating procedures, 32 (74.4%) were in private
gynecology sector and 11 (25.5%) in public sector. No statistically significant
Dentistry 04 (50.0%) 04 (50.0% 08 (2.5%) difference was found in these two groups in terms of deliberate
Others (anesthesia) 19 (55.8%) 15 (44.1%) 34 (10.6%) lessening of aerosol-generating procedures (p = 0.46). Fifteen
224 (70.4%) 94 (29.5%) 318 (100%) (63.5%) participants from private sector have deferred surgery
Table 3: Distribution of the respondents according to infrastructure and SOP preparedness for surgical interventions during COVID-19
Private sector Public sector
Infrastructure and SOPs preparedness for COVID-19 respondent (n = 238) respondents (n = 80) OR (CI) p value
Standard protocol and triage for COVID-19 at workplace (n = 166), 132 (79.5%) 34 (20.4%) 1.68 (1.01–2.81) 0.02
i.e., 52.2%
Dedicated COVID-19 recovery and wards (n = 143), i.e., 44.9% 118 (82.5%) 25 (17.4%) 2.16 (1.27–3.70) 0.006
Negative-pressure operation theaters and anterooms (n = 34), 29 (85.2%) 5 (14.7%) 2.08 (0.77–5.57) 0.2
i.e., 10.6%
Separate paramedical and axillary staff for operating COVID-19 14 (93.3%) 1 (6.7%) 4.9 (0.6–38.2) 0.07
patients (n =15), i.e., 4.7%
Have verified the correct procedure and sequence for donning and 163 (75.1%) 54 (24.8%) 1.04 (0.60–1.79) 0.43
doffing PPE (n = 217), i.e., 68.2%
Impaired vision due to fogging N = (198) 62.2% 147 (%) 51 (%) 0.91 (0.54–1.55) 0.42
World Journal of Laparoscopic Surgery, Volume 14 Issue 3 (September–December 2021) 187