Page 64 - tmp
P. 64
Gastric Remnant Perforation after Roux-en-Y Gastric Bypass
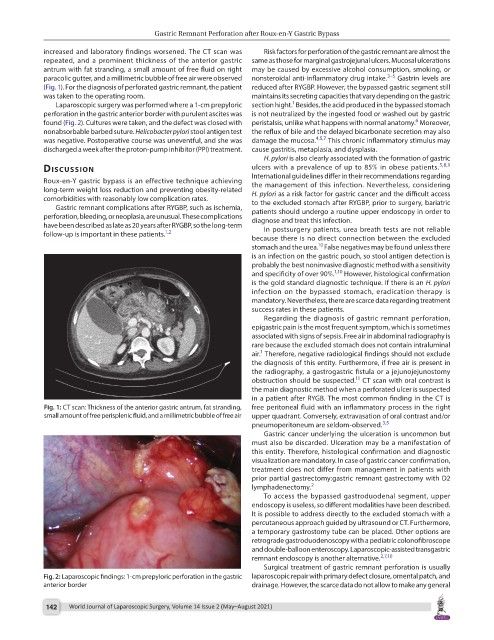
increased and laboratory findings worsened. The CT scan was Risk factors for perforation of the gastric remnant are almost the
repeated, and a prominent thickness of the anterior gastric same as those for marginal gastrojejunal ulcers. Mucosal ulcerations
antrum with fat stranding, a small amount of free fluid on right may be caused by excessive alcohol consumption, smoking, or
paracolic gutter, and a millimetric bubble of free air were observed nonsteroidal anti-inflammatory drug intake. 3–5 Gastrin levels are
(Fig. 1). For the diagnosis of perforated gastric remnant, the patient reduced after RYGBP. However, the bypassed gastric segment still
was taken to the operating room. maintains its secreting capacities that vary depending on the gastric
1
Laparoscopic surgery was performed where a 1-cm prepyloric section hight. Besides, the acid produced in the bypassed stomach
perforation in the gastric anterior border with purulent ascites was is not neutralized by the ingested food or washed out by gastric
6
found (Fig. 2). Cultures were taken, and the defect was closed with peristalsis, unlike what happens with normal anatomy. Moreover,
nonabsorbable barbed suture. Helicobacter pylori stool antigen test the reflux of bile and the delayed bicarbonate secretion may also
was negative. Postoperative course was uneventful, and she was damage the mucosa. 4,5,7 This chronic inflammatory stimulus may
discharged a week after the proton-pump inhibitor (PPI) treatment. cause gastritis, metaplasia, and dysplasia.
H. pylori is also clearly associated with the formation of gastric
discussion ulcers with a prevalence of up to 85% in obese patients. 5,8,9
Roux-en-Y gastric bypass is an effective technique achieving International guidelines differ in their recommendations regarding
the management of this infection. Nevertheless, considering
long-term weight loss reduction and preventing obesity-related H. pylori as a risk factor for gastric cancer and the difficult access
comorbidities with reasonably low complication rates. to the excluded stomach after RYGBP, prior to surgery, bariatric
Gastric remnant complications after RYGBP, such as ischemia, patients should undergo a routine upper endoscopy in order to
perforation, bleeding, or neoplasia, are unusual. These complications diagnose and treat this infection.
have been described as late as 20 years after RYGBP, so the long-term In postsurgery patients, urea breath tests are not reliable
follow-up is important in these patients. 1,2
because there is no direct connection between the excluded
10
stomach and the urea. False negatives may be found unless there
is an infection on the gastric pouch, so stool antigen detection is
probably the best noninvasive diagnostic method with a sensitivity
and specificity of over 90%. 1,10 However, histological confirmation
is the gold standard diagnostic technique. If there is an H. pylori
infection on the bypassed stomach, eradication therapy is
mandatory. Nevertheless, there are scarce data regarding treatment
success rates in these patients.
Regarding the diagnosis of gastric remnant perforation,
epigastric pain is the most frequent symptom, which is sometimes
associated with signs of sepsis. Free air in abdominal radiography is
rare because the excluded stomach does not contain intraluminal
1
air. Therefore, negative radiological findings should not exclude
the diagnosis of this entity. Furthermore, if free air is present in
the radiography, a gastrogastric fistula or a jejunojejunostomy
11
obstruction should be suspected. CT scan with oral contrast is
the main diagnostic method when a perforated ulcer is suspected
in a patient after RYGB. The most common finding in the CT is
Fig. 1: CT scan: Thickness of the anterior gastric antrum, fat stranding, free peritoneal fluid with an inflammatory process in the right
small amount of free perisplenic fluid, and a millimetric bubble of free air upper quadrant. Conversely, extravasation of oral contrast and/or
pneumoperitoneum are seldom-observed. 3,5
Gastric cancer underlying the ulceration is uncommon but
must also be discarded. Ulceration may be a manifestation of
this entity. Therefore, histological confirmation and diagnostic
visualization are mandatory. In case of gastric cancer confirmation,
treatment does not differ from management in patients with
prior partial gastrectomy:gastric remnant gastrectomy with D2
lymphadenectomy. 2
To access the bypassed gastroduodenal segment, upper
endoscopy is useless, so different modalities have been described.
It is possible to address directly to the excluded stomach with a
percutaneous approach guided by ultrasound or CT. Furthermore,
a temporary gastrostomy tube can be placed. Other options are
retrograde gastroduodenoscopy with a pediatric colonofibroscope
and double-balloon enteroscopy. Laparoscopic-assisted transgastric
remnant endoscopy is another alternative. 2,7,10
Surgical treatment of gastric remnant perforation is usually
Fig. 2: Laparoscopic findings: 1-cm prepyloric perforation in the gastric laparoscopic repair with primary defect closure, omental patch, and
anterior border drainage. However, the scarce data do not allow to make any general
142 World Journal of Laparoscopic Surgery, Volume 14 Issue 2 (May–August 2021)