Page 43 - tmp
P. 43
Gastric Cancer Resection
The patients were followed up for 30 days. Hospital stay
was increased nonsignificantly among OG group 8.0 ± 4.1 days
compared to LG group 6.9 ± 2.6 days (p-value = 0.361). Time to
first flatus was nonsignificantly longer in OG group (2.4 ± 0.51 days)
compared to LG group (2.5 ± 0.52 days) with p value = 0.773
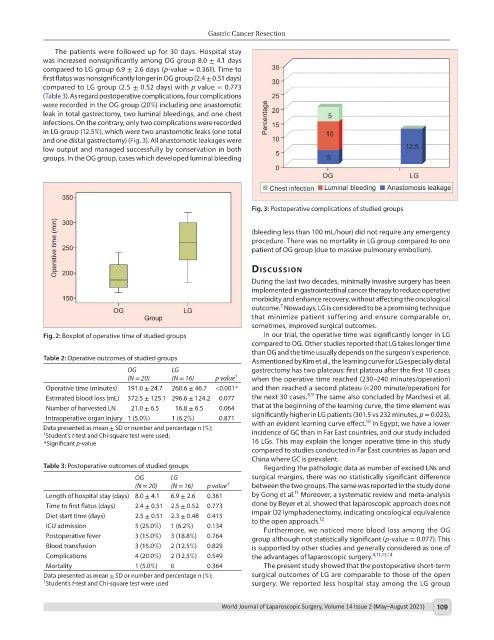
(Table 3). As regard postoperative complications, four complications
were recorded in the OG group (20%) including one anastomotic
leak in total gastrectomy, two luminal bleedings, and one chest
infections. On the contrary, only two complications were recorded
in LG group (12.5%), which were two anastomotic leaks (one total
and one distal gastrectomy) (Fig. 3). All anastomotic leakages were
low output and managed successfully by conservation in both
groups. In the OG group, cases which developed luminal bleeding
Fig. 3: Postoperative complications of studied groups
(bleeding less than 100 mL/hour) did not require any emergency
procedure. There was no mortality in LG group compared to one
patient of OG group (due to massive pulmonary embolism).
dIscussIon
During the last two decades, minimally invasive surgery has been
implemented in gastrointestinal cancer therapy to reduce operative
morbidity and enhance recovery, without affecting the oncological
7
outcome. Nowadays, LG is considered to be a promising technique
that minimize patient suffering and ensure comparable or,
sometimes, improved surgical outcomes.
Fig. 2: Boxplot of operative time of studied groups In our trial, the operative time was significantly longer in LG
compared to OG. Other studies reported that LG takes longer time
than OG and the time usually depends on the surgeon’s experience.
Table 2: Operative outcomes of studied groups As mentioned by Kim et al., the learning curve for LG especially distal
OG LG gastrectomy has two plateaus: first plateau after the first 10 cases
(N = 20) (N = 16) p value † when the operative time reached (230–240 minutes/operation)
Operative time (minutes) 191.0 ± 24.7 260.6 ± 46.7 <0.001* and then reached a second plateau (<200 minute/operation) for
8,9
Estimated blood loss (mL) 372.5 ± 125.1 296.6 ± 124.2 0.077 the next 30 cases. The same also concluded by Marchesi et al.
Number of harvested LN 21.0 ± 6.5 16.8 ± 6.5 0.064 that at the beginning of the learning curve, the time element was
Intraoperative organ injury 1 (5.0%) 1 (6.2%) 0.871 significantly higher in LG patients (301.5 vs 232 minutes, p = 0.023),
10
Data presented as mean ± SD or number and percentage n (%); with an evident learning curve effect. In Egypt, we have a lower
Student’s t-test and Chi-square test were used;
† incidence of GC than in Far East countries, and our study included
*Significant p-value 16 LGs. This may explain the longer operative time in this study
compared to studies conducted in Far East countries as Japan and
China where GC is prevalent.
Table 3: Postoperative outcomes of studied groups Regarding the pathologic data as number of excised LNs and
OG LG surgical margins, there was no statistically significant difference
(N = 20) (N = 16) p value † between the two groups. The same was reported in the study done
11
Length of hospital stay (days) 8.0 ± 4.1 6.9 ± 2.6 0.361 by Gong et al. Moreover, a systematic review and meta-analysis
Time to first flatus (days) 2.4 ± 0.51 2.5 ± 0.52 0.773 done by Beyer et al. showed that laparoscopic approach does not
Diet start time (days) 2.5 ± 0.51 2.3 ± 0.48 0.415 impair D2 lymphadenectomy, indicating oncological equivalence
12
to the open approach.
ICU admission 5 (25.0%) 1 (6.2%) 0.134 Furthermore, we noticed more blood loss among the OG
Postoperative fever 3 (15.0%) 3 (18.8%) 0.764 group although not statistically significant (p-value = 0.077). This
Blood transfusion 3 (15.0%) 2 (12.5%) 0.829 is supported by other studies and generally considered as one of
Complications 4 (20.0%) 2 (12.5%) 0.549 the advantages of laparoscopic surgery. 4,11,13,14
Mortality 1 (5.0%) 0 0.364 The present study showed that the postoperative short-term
Data presented as mean ± SD or number and percentage n (%); surgical outcomes of LG are comparable to those of the open
† Student’s t-test and Chi-square test were used surgery. We reported less hospital stay among the LG group
World Journal of Laparoscopic Surgery, Volume 14 Issue 2 (May–August 2021) 109