Page 5 - World Journal of Laparoscopic Surgery
P. 5
Laparoscopic Appendicectomy and Complicated Appendicitis
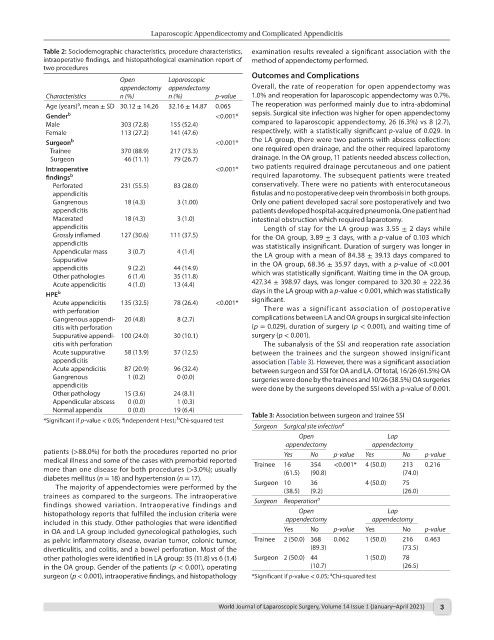
Table 2: Sociodemographic characteristics, procedure characteristics, examination results revealed a significant association with the
intraoperative findings, and histopathological examination report of method of appendectomy performed.
two procedures
Open Laparoscopic Outcomes and Complications
appendectomy appendectomy Overall, the rate of reoperation for open appendectomy was
Characteristics n (%) n (%) p-value 1.0% and reoperation for laparoscopic appendectomy was 0.7%.
a
Age (years) , mean ± SD 30.12 ± 14.26 32.16 ± 14.87 0.065 The reoperation was performed mainly due to intra-abdominal
Gender b <0.001* sepsis. Surgical site infection was higher for open appendectomy
Male 303 (72.8) 155 (52.4) compared to laparoscopic appendectomy, 26 (6.3%) vs 8 (2.7),
Female 113 (27.2) 141 (47.6) respectively, with a statistically significant p-value of 0.029. In
Surgeon b <0.001* the LA group, there were two patients with abscess collection:
Trainee 370 (88.9) 217 (73.3) one required open drainage, and the other required laparotomy
Surgeon 46 (11.1) 79 (26.7) drainage. In the OA group, 11 patients needed abscess collection,
Intraoperative <0.001* two patients required drainage percutaneous and one patient
findings b required laparotomy. The subsequent patients were treated
Perforated 231 (55.5) 83 (28.0) conservatively. There were no patients with enterocutaneous
appendicitis fistulas and no postoperative deep vein thrombosis in both groups.
Gangrenous 18 (4.3) 3 (1.00) Only one patient developed sacral sore postoperatively and two
appendicitis patients developed hospital-acquired pneumonia. One patient had
Macerated 18 (4.3) 3 (1.0) intestinal obstruction which required laparotomy.
appendicitis Length of stay for the LA group was 3.55 ± 2 days while
Grossly inflamed 127 (30.6) 111 (37.5) for the OA group, 3.89 ± 3 days, with a p-value of 0.103 which
appendicitis was statistically insignificant. Duration of surgery was longer in
Appendicular mass 3 (0.7) 4 (1.4) the LA group with a mean of 84.38 ± 39.13 days compared to
Suppurative in the OA group, 68.36 ± 35.97 days, with a p-value of <0.001
appendicitis 9 (2.2) 44 (14.9)
Other pathologies 6 (1.4) 35 (11.8) which was statistically significant. Waiting time in the OA group,
Acute appendicitis 4 (1.0) 13 (4.4) 427.34 ± 398.97 days, was longer compared to 320.30 ± 222.36
HPE b days in the LA group with a p-value < 0.001, which was statistically
Acute appendicitis 135 (32.5) 78 (26.4) <0.001* significant.
with perforation There was a significant association of postoperative
Gangrenous appendi- 20 (4.8) 8 (2.7) complications between LA and OA groups in surgical site infection
citis with perforation (p = 0.029), duration of surgery (p < 0.001), and waiting time of
Suppurative appendi- 100 (24.0) 30 (10.1) surgery (p < 0.001).
citis with perforation The subanalysis of the SSI and reoperation rate association
Acute suppurative 58 (13.9) 37 (12.5) between the trainees and the surgeon showed insignificant
appendicitis association (Table 3). However, there was a significant association
Acute appendicitis 87 (20.9) 96 (32.4) between surgeon and SSI for OA and LA. Of total, 16/26 (61.5%) OA
Gangrenous 1 (0.2) 0 (0.0) surgeries were done by the trainees and 10/26 (38.5%) OA surgeries
appendicitis were done by the surgeons developed SSI with a p-value of 0.001.
Other pathology 15 (3.6) 24 (8.1)
Appendicular abscess 0 (0.0) 1 (0.3)
Normal appendix 0 (0.0) 19 (6.4)
b
a
*Significant if p-value < 0.05; Independent t-test; Chi-squared test Table 3: Association between surgeon and trainee SSI
Surgeon Surgical site infection a
Open Lap
appendectomy appendectomy
patients (>88.0%) for both the procedures reported no prior Yes No p-value Yes No p-value
medical illness and some of the cases with premorbid reported Trainee 16 354 <0.001* 4 (50.0) 213 0.216
more than one disease for both procedures (>3.0%); usually (61.5) (90.8) (74.0)
diabetes mellitus (n = 18) and hypertension (n = 17).
The majority of appendectomies were performed by the Surgeon 10 36 4 (50.0) 75
(9.2)
(38.5)
(26.0)
trainees as compared to the surgeons. The intraoperative a
findings showed variation. Intraoperative findings and Surgeon Reoperation
histopathology reports that fulfilled the inclusion criteria were Open Lap
included in this study. Other pathologies that were identified appendectomy appendectomy
in OA and LA group included gynecological pathologies, such Yes No p-value Yes No p-value
as pelvic inflammatory disease, ovarian tumor, colonic tumor, Trainee 2 (50.0) 368 0.062 1 (50.0) 216 0.463
diverticulitis, and colitis, and a bowel perforation. Most of the (89.3) (73.5)
other pathologies were identified in LA group: 35 (11.8) vs 6 (1.4) Surgeon 2 (50.0) 44 1 (50.0) 78
in the OA group. Gender of the patients (p < 0.001), operating (10.7) (26.5)
a
surgeon (p < 0.001), intraoperative findings, and histopathology *Significant if p-value < 0.05; Chi-squared test
World Journal of Laparoscopic Surgery, Volume 14 Issue 1 (January–April 2021) 3