Page 42 - World Journal of Laparoscopic Surgery
P. 42
Innovative Technique to Control the COVID‑19 Transmission by Surgical Fume
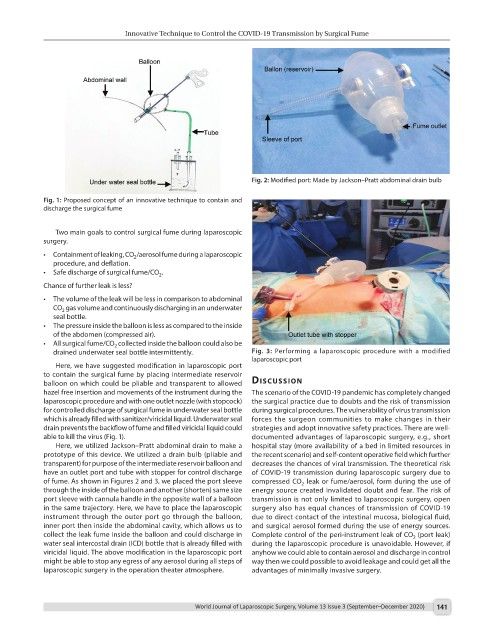
Fig. 2: Modified port: Made by Jackson–Pratt abdominal drain bulb
Fig. 1: Proposed concept of an innovative technique to contain and
discharge the surgical fume
Two main goals to control surgical fume during laparoscopic
surgery.
• Containment of leaking, CO /aerosol fume during a laparoscopic
2
procedure, and deflation.
• Safe discharge of surgical fume/CO .
2
Chance of further leak is less?
• The volume of the leak will be less in comparison to abdominal
CO gas volume and continuously discharging in an underwater
2
seal bottle.
• The pressure inside the balloon is less as compared to the inside
of the abdomen (compressed air).
• All surgical fume/CO collected inside the balloon could also be
2
drained underwater seal bottle intermittently. Fig. 3: Performing a laparoscopic procedure with a modified
laparoscopic port
Here, we have suggested modification in laparoscopic port
to contain the surgical fume by placing intermediate reservoir
balloon on which could be pliable and transparent to allowed discussion
hazel free insertion and movements of the instrument during the The scenario of the COVID-19 pandemic has completely changed
laparoscopic procedure and with one outlet nozzle (with stopcock) the surgical practice due to doubts and the risk of transmission
for controlled discharge of surgical fume in underwater seal bottle during surgical procedures. The vulnerability of virus transmission
which is already filled with sanitizer/viricidal liquid. Underwater seal forces the surgeon communities to make changes in their
drain prevents the backflow of fume and filled viricidal liquid could strategies and adopt innovative safety practices. There are well-
able to kill the virus (Fig. 1). documented advantages of laparoscopic surgery, e.g., short
Here, we utilized Jackson–Pratt abdominal drain to make a hospital stay (more availability of a bed in limited resources in
prototype of this device. We utilized a drain bulb (pliable and the recent scenario) and self-content operative field which further
transparent) for purpose of the intermediate reservoir balloon and decreases the chances of viral transmission. The theoretical risk
have an outlet port and tube with stopper for control discharge of COVID-19 transmission during laparoscopic surgery due to
of fume. As shown in Figures 2 and 3, we placed the port sleeve compressed CO leak or fume/aerosol, form during the use of
2
through the inside of the balloon and another (shorten) same size energy source created invalidated doubt and fear. The risk of
port sleeve with cannula handle in the opposite wall of a balloon transmission is not only limited to laparoscopic surgery, open
in the same trajectory. Here, we have to place the laparoscopic surgery also has equal chances of transmission of COVID-19
instrument through the outer port go through the balloon, due to direct contact of the intestinal mucosa, biological fluid,
inner port then inside the abdominal cavity, which allows us to and surgical aerosol formed during the use of energy sources.
collect the leak fume inside the balloon and could discharge in Complete control of the peri-instrument leak of CO (port leak)
2
water seal intercostal drain (ICD) bottle that is already filled with during the laparoscopic procedure is unavoidable. However, if
viricidal liquid. The above modification in the laparoscopic port anyhow we could able to contain aerosol and discharge in control
might be able to stop any egress of any aerosol during all steps of way then we could possible to avoid leakage and could get all the
laparoscopic surgery in the operation theater atmosphere. advantages of minimally invasive surgery.
World Journal of Laparoscopic Surgery, Volume 13 Issue 3 (September–December 2020) 141