Page 38 - WJOLS
P. 38
Rooh-ul-Muqim et al
hernia and to rule out any strangulation, etc. Routine base line patients had paraumbilical hernia, 9 (16.66%) had epigastric
investigations like full blood count, blood glucose level, urina- and 7 (12.96%) had umbilical hernia. Umbilical and paraumbilical
lysis and hepatitis screen were done in all patients. An abdo- hernias were small ranging from 2-5 cm defect. The incisional
minal ultrasonography was done to the exclude any other hernia ranged from 5-10 cm while in only 2 (3.20%) patients
pathology like gallstones or any other intra-abdominal patho- defects was greater than 10 cm in size (Table 2). Incisional hernias
logy. The patient was counseled regarding the procedure and a of the upper middle and lower middle scars were 5 (9.25%) each
written consent was obtained. The laparoscopic mesh repair while 6 (11.11%) occurred after suprapubic (pfaunenstiel)
was performed under general anesthesia. The patient was incision.
positioned according to the site of hernia. Only 2 ports for laparoscopic repair were used in 22 patients,
in 19 patients 3 ports were used whereas in 3 patients with big
TECHNIQUE hernias a 4th port was also introduced. In all patients proline
mesh was used. In all patients the procedure was successfully
Two or three and sometimes four ports were used depending completed laparoscopically. No additional procedure were
on the hernia, using base ball diamond concept. Adhesiolysis carried out during herniorrhaphy. Intraoperative blood loss was
was performed and contents of the sac were released and negligible. The duration of operation was 35 minutes to
reduced. The defect was identified and proline mesh was 2 hours. The postoperative stay in hospital ranged from 1-3
measured on the defect from the outside. Sutures were applied days (Table 3).
at three corners of the mesh using vicryl 1or 0 suture, and both
the ends of the suture were left long and cut at 6-10 cm length
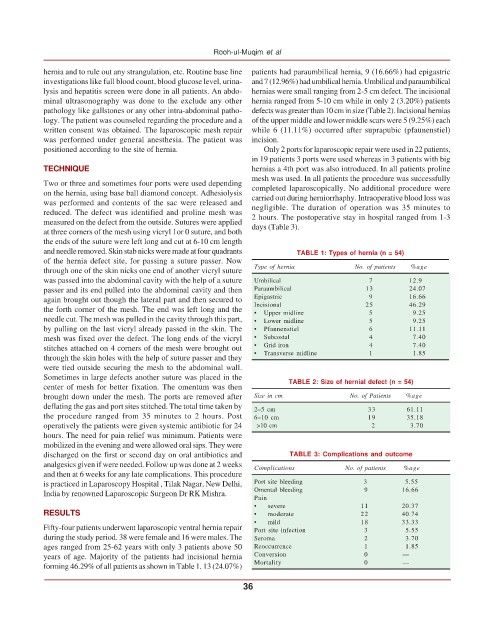
and needle removed. Skin stab nicks were made at four quadrants TABLE 1: Types of hernia (n = 54)
of the hernia defect site, for passing a suture passer. Now
through one of the skin nicks one end of another vicryl suture Type of hernia No. of patients %age
was passed into the abdominal cavity with the help of a suture Umbilical 7 12.9
passer and its end pulled into the abdominal cavity and then Paraumbilical 13 24.07
again brought out though the lateral part and then secured to Epigastric 9 16.66
the forth corner of the mesh. The end was left long and the Incisional 25 5 46.29
Upper midline
9.25
•
needle cut. The mesh was pulled in the cavity through this part, • Lower midline 5 9.25
by pulling on the last vicryl already passed in the skin. The • Pfannenstiel 6 11.11
mesh was fixed over the defect. The long ends of the vicryl • Subcostal 4 7.40
stitches attached on 4 corners of the mesh were brought out • Grid iron 4 7.40
through the skin holes with the help of suture passer and they • Transverse midline 1 1.85
were tied outside securing the mesh to the abdominal wall.
Sometimes in large defects another suture was placed in the
center of mesh for better fixation. The omentum was then TABLE 2: Size of hernial defect (n = 54)
brought down under the mesh. The ports are removed after Size in cm No. of Patients %age
deflating the gas and port sites stitched. The total time taken by 2–5 cm 33 61.11
the procedure ranged from 35 minutes to 2 hours. Post 6–10 cm 19 35.18
operatively the patients were given systemic antibiotic for 24 >10 cm 2 3.70
hours. The need for pain relief was minimum. Patients were
mobilized in the evening and were allowed oral sips. They were
discharged on the first or second day on oral antibiotics and TABLE 3: Complications and outcome
analgesics given if were needed. Follow up was done at 2 weeks Complications No. of patients %age
and then at 6 weeks for any late complications. This procedure
is practiced in Laparoscopy Hospital , Tilak Nagar, New Delhi, Port site bleeding 3 5.55
India by renowned Laparoscopic Surgeon Dr RK Mishra. Omental bleeding 9 16.66
Pain
• severe 11 20.37
RESULTS • moderate 22 40.74
• mild 18 33.33
Fifty-four patients underwent laparoscopic ventral hernia repair Port site infection 3 5.55
during the study period. 38 were female and 16 were males. The Seroma 2 3.70
ages ranged from 25-62 years with only 3 patients above 50 Reoccurrence 1 1.85
years of age. Majority of the patients had incisional hernia Conversion 0 —
forming 46.29% of all patients as shown in Table 1. 13 (24.07%) Mortality 0 —
36