Page 49 - World Journal of Laparoscopic Surgery
P. 49
CASE REPORT
Portomesenteric Venous Thrombosis with Bowel Ischemia
after Laparoscopic Sleeve Gastrectomy
3
4
1
2
Mubarak Alkandari , Samir Abdulaziz , Mohamed Alsulimy , Nagy Ismaeil , Mohamed Mohsen 5
AbstrAct
Laparoscopic sleeve gastrectomy has become an increasingly popular surgical option for morbidly obese patients. Portomesenteric venous
thrombosis, as a complication of laparoscopic sleeve gastrectomy, has been rarely reported. We report one case of thrombosis of the portal
vein and the superior mesenteric vein after sleeve gastrectomy. It is confirmed by CT scan. Thrombosis of the portomesenteric veins after
bariatric surgery is a diagnosis that one should know how to raise in front of any postoperative abdominal pain. An obese patient with a history
of thrombosis should receive a complete etiology of these thromboses before bariatric surgery. Abnormal blood dirt, an active smoking fat
woman having oral contraceptive, or a patient with a history of recurrent venous thrombosis may be a relative contraindication against a
complex bariatric surgery with digestive bypass.
Keywords: Bowel ischemia, Diagnostic laparoscopy, Laparoscopic sleeve gastrectomy.
World Journal of Laparoscopic Surgery (2019): 10.5005/jp-journals-10033-1385
IntroductIon 1–5 Department of Surgery, Al-Sabah Hospital, Kuwait
Bariatric surgery is being used with increased frequency for effective Corresponding Author: Mohamed Mohsen, Department of
1
weight loss in patient with morbid obesity. However, although Surgery, Al-Sabah Hospital, Kuwait, Phone: +965 60463440, e-mail:
rare, life-threatening complications such as mesenteric ischemia mohsenroom@yahoo.com
2
and pulmonary embolism occur. The incidence of deep vein How to cite this article: Alkandari M, Abdulaziz S, Alsulimy M, et al.
3
thrombosis (DVT) after bariatric surgery varies from 1.2 to 1.6%. Portomesenteric Venous Thrombosis with Bowel Ischemia after
Portomesenteric venous thrombosis (PMVT) is a rare vascular event Laparoscopic Sleeve Gastrectomy. World J Lap Surg 2019;12(3):135–137.
but is associated with high mortality rates (20–45%). 3,4 Source of support: Nil
Conflict of interest: None
cAse descrIptIon
A 35-year-old patient underwent a laparoscopic sleeve gastrectomy
2
for the treatment of obesity (BMI 41 kg/m ). The patient was He was discharged on the 7th postoperative day. Pre- and
not a smoker and she was not having any chronic debilitated postoperative activated partial thromboplastin time (aPTT)
diseases. The surgical procedure was simple with an operative and international normalized ratio (INR) values were observed;
time of 45 minutes. The immediate postoperative course was other blood tests, protein C and S deficiency, and phospholipid
simple and uneventful, and the hospitalization ended on the 3rd enzymes assessment had been requested. The patient underwent
day. The patient was again admitted to emergency on the 14th in the postoperative hospitalization period low molecular weight
postoperative day for severe epigastric abdominal pain associated
with nausea and persistent repeated vomiting of 2 days’ duration.
On examination, she was vitally stable with BP: 110/60 mmHg, temp.:
36.8°C, and pulse: 90b/m. The abdomen was tender with guarding,
while the patient was tachycardic but febrile. X-ray abdomen
showed dilated small bowel loops. The investigations were found
without abnormalities apart from positive ketonuria and high serum
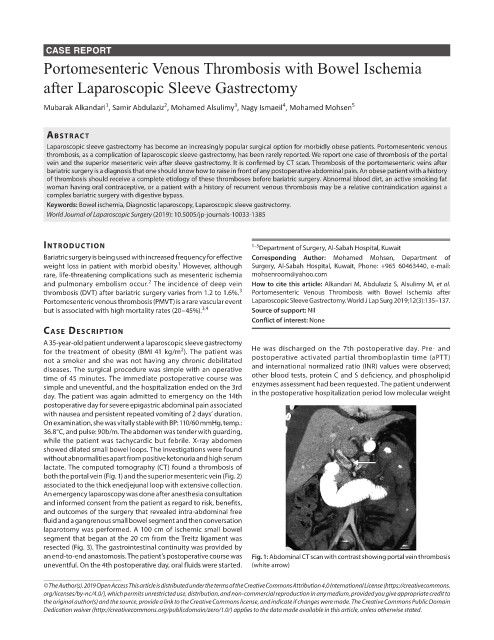
lactate. The computed tomography (CT) found a thrombosis of
both the portal vein (Fig. 1) and the superior mesenteric vein (Fig. 2)
associated to the thick enedjejunal loop with extensive collection.
An emergency laparoscopy was done after anesthesia consultation
and informed consent from the patient as regard to risk, benefits,
and outcomes of the surgery that revealed intra-abdominal free
fluid and a gangrenous small bowel segment and then conversation
laparotomy was performed. A 100 cm of ischemic small bowel
segment that began at the 20 cm from the Treitz ligament was
resected (Fig. 3). The gastrointestinal continuity was provided by
an end-to-end anastomosis. The patient’s postoperative course was Fig. 1: Abdominal CT scan with contrast showing portal vein thrombosis
uneventful. On the 4th postoperative day, oral fluids were started. (white arrow)
© The Author(s). 2019 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.
org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to
the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain
Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.