Page 22 - World Association of Laparoscopic Surgeons - Journal
P. 22
WJOLS
Role of Falloposcopy in the Management of Subfertility
the tubal ostium can be visualized in the absence of blood space (the balloon space) is controlled by a fluid-filled
and thick endometrium. However, prior to the procedure syringe. The falloposcopy is advanced within the inner
an informed consent is taken from the patient. The process catheter and the membrane is introduced into the uterus.
takes 30 to 40 minutes, but if a minor tubal surgery will be Once the ostium is identified, the outer catheter is held in
performed it takes an average of 1 to 2 and half hours. It is position and pressure is applied to the membrane by using
usually done under conscious sedation but if one is the fluid-filled syringe; the inner catheter is pushed forward,
proceeding to tubal surgery then it is converted to general resulting in the linear eversion of the balloon into the
anesthesia. A prophylactic antibiotic is not a prerequisite fallopian tube.
to the procedure. The balloon and falloposcope are advanced into the
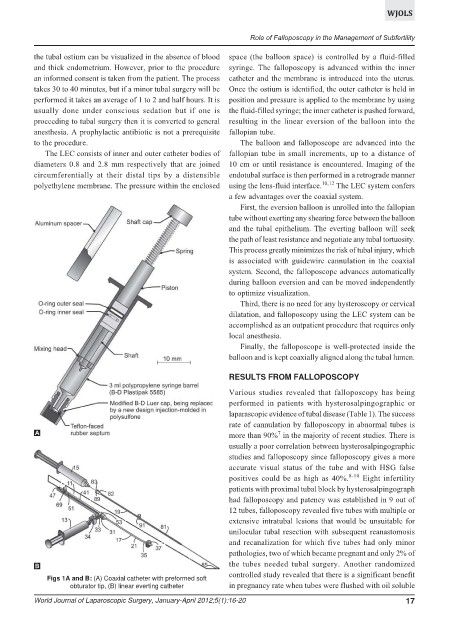
The LEC consists of inner and outer catheter bodies of fallopian tube in small increments, up to a distance of
diameters 0.8 and 2.8 mm respectively that are joined 10 cm or until resistance is encountered. Imaging of the
circumferentially at their distal tips by a distensible endotubal surface is then performed in a retrograde manner
polyethylene membrane. The pressure within the enclosed using the lens-fluid interface. 10,12 The LEC system confers
a few advantages over the coaxial system.
First, the eversion balloon is unrolled into the fallopian
tube without exerting any shearing force between the balloon
and the tubal epithelium. The everting balloon will seek
the path of least resistance and negotiate any tubal tortuosity.
This process greatly minimizes the risk of tubal injury, which
is associated with guidewire cannulation in the coaxial
system. Second, the falloposcope advances automatically
during balloon eversion and can be moved independently
to optimize visualization.
Third, there is no need for any hysteroscopy or cervical
dilatation, and falloposcopy using the LEC system can be
accomplished as an outpatient procedure that requires only
local anesthesia.
Finally, the falloposcope is well-protected inside the
balloon and is kept coaxially aligned along the tubal lumen.
RESULTS FROM FALLOPOSCOPY
Various studies revealed that falloposcopy has being
performed in patients with hysterosalpingographic or
laparascopic evidence of tubal disease (Table 1). The success
rate of cannulation by falloposcopy in abnormal tubes is
A 7
more than 90% in the majority of recent studies. There is
usually a poor correlation between hysterosalpingographic
studies and falloposcopy since falloposcopy gives a more
accurate visual status of the tube and with HSG false
positives could be as high as 40%. 8-10 Eight infertility
patients with proximal tubal block by hysterosalpingograph
had falloposcopy and patency was established in 9 out of
12 tubes, falloposcopy revealed five tubes with multiple or
extensive intratubal lesions that would be unsuitable for
unilocular tubal resection with subsequent reanastomosis
and recanalization for which five tubes had only minor
pathologies, two of which became pregnant and only 2% of
B the tubes needed tubal surgery. Another randomized
controlled study revealed that there is a significant benefit
Figs 1A and B: (A) Coaxial catheter with preformed soft
obturator tip, (B) linear everting catheter in pregnancy rate when tubes were flushed with oil soluble
World Journal of Laparoscopic Surgery, January-April 2012;5(1):16-20 17