Page 5 - Jourmal of World Association of Laparoscopic Surgeon
P. 5
WJOLS
Veress Needle: A Safe Technique in Modern Laparoscopic Era
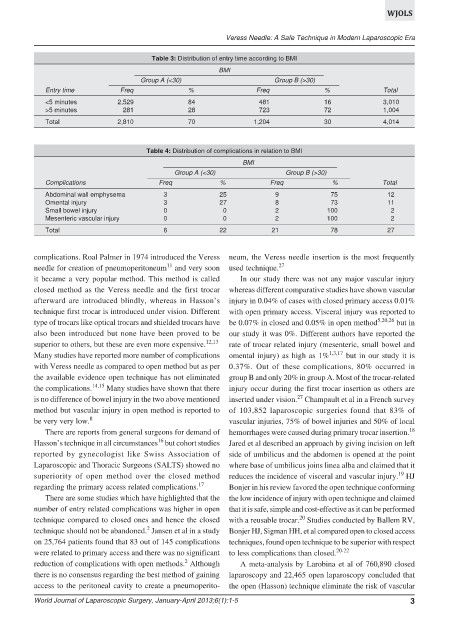
Table 3: Distribution of entry time according to BMI
BMI
Group A (<30) Group B (>30)
Entry time Freq % Freq % Total
<5 minutes 2,529 84 481 16 3,010
>5 minutes 281 28 723 72 1,004
Total 2,810 70 1,204 30 4,014
Table 4: Distribution of complications in relation to BMI
BMI
Group A (<30) Group B (>30)
Complications Freq % Freq % Total
Abdominal wall emphysema 3 25 9 75 12
Omental injury 3 27 8 73 11
Small bowel injury 0 0 2 100 2
Mesenteric vascular injury 0 0 2 100 2
Total 6 22 21 78 27
complications. Roal Palmer in 1974 introduced the Veress neum, the Veress needle insertion is the most frequently
11
needle for creation of pneumoperitoneum and very soon used technique. 27
it became a very popular method. This method is called In our study there was not any major vascular injury
closed method as the Veress needle and the first trocar whereas different comparative studies have shown vascular
afterward are introduced blindly, whereas in Hasson’s injury in 0.04% of cases with closed primary access 0.01%
technique first trocar is introduced under vision. Different with open primary access. Visceral injury was reported to
type of trocars like optical trocars and shielded trocars have be 0.07% in closed and 0.05% in open method 5,20,26 but in
also been introduced but none have been proved to be our study it was 0%. Different authors have reported the
superior to others, but these are even more expensive. 12,13 rate of trocar related injury (mesenteric, small bowel and
Many studies have reported more number of complications omental injury) as high as 1% 1,3,17 but in our study it is
with Veress needle as compared to open method but as per 0.37%. Out of these complications, 80% occurred in
the available evidence open technique has not eliminated group B and only 20% in group A. Most of the trocar-related
the complications. 14,15 Many studies have shown that there injury occur during the first trocar insertion as others are
27
is no difference of bowel injury in the two above mentioned inserted under vision. Champault et al in a French survey
method but vascular injury in open method is reported to of 103,852 laparoscopic surgeries found that 83% of
be very very low. 8 vascular injuries, 75% of bowel injuries and 50% of local
There are reports from general surgeons for demand of hemorrhages were caused during primary trocar insertion. 18
16
Hasson’s technique in all circumstances but cohort studies Jared et al described an approach by giving incision on left
reported by gynecologist like Swiss Association of side of umbilicus and the abdomen is opened at the point
Laparoscopic and Thoracic Surgeons (SALTS) showed no where base of umbilicus joins linea alba and claimed that it
19
superiority of open method over the closed method reduces the incidence of visceral and vascular injury. HJ
regarding the primary access related complications. 17 Bonjer in his review favored the open technique conforming
There are some studies which have highlighted that the the low incidence of injury with open technique and claimed
number of entry related complications was higher in open that it is safe, simple and cost-effective as it can be performed
20
technique compared to closed ones and hence the closed with a reusable trocar. Studies conducted by Ballem RV,
2
technique should not be abandoned. Jansen et al in a study Bonjer HJ, Sigman HH, et al compared open to closed access
on 25,764 patients found that 83 out of 145 complications techniques, found open technique to be superior with respect
were related to primary access and there was no significant to less complications than closed. 20-22
2
reduction of complications with open methods. Although A meta-analysis by Larobina et al of 760,890 closed
there is no consensus regarding the best method of gaining laparoscopy and 22,465 open laparoscopy concluded that
access to the peritoneal cavity to create a pneumoperito- the open (Hasson) technique eliminate the risk of vascular
World Journal of Laparoscopic Surgery, January-April 2013;6(1):1-5 3