Page 15 - Jourmal of World Association of Laparoscopic Surgeon
P. 15
WJOLS
A Comparative Study of Laparoscopic vs Open Surgery for the Management of Duodenal Ulcer Perforation
A B
Figs 3A and B: Perforation closed by placing omentum
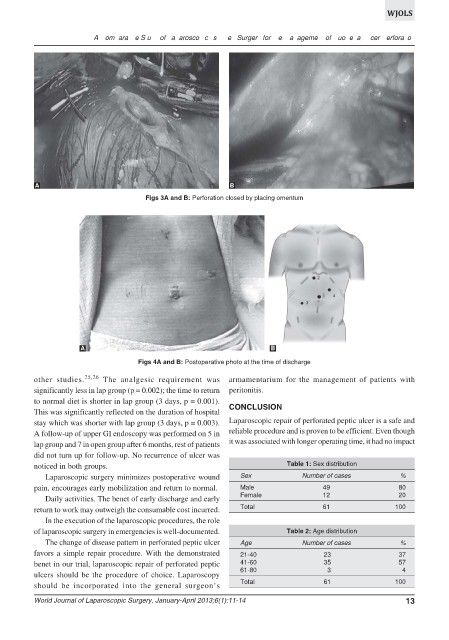
A B
Figs 4A and B: Postoperative photo at the time of discharge
other studies. 25,26 The analgesic requirement was armamentarium for the management of patients with
significantly less in lap group (p = 0.002); the time to return peritonitis.
to normal diet is shorter in lap group (3 days, p = 0.001).
This was significantly reflected on the duration of hospital CONCLUSION
stay which was shorter with lap group (3 days, p = 0.003). Laparoscopic repair of perforated peptic ulcer is a safe and
A follow-up of upper GI endoscopy was performed on 5 in reliable procedure and is proven to be efficient. Even though
lap group and 7 in open group after 6 months, rest of patients it was associated with longer operating time, it had no impact
did not turn up for follow-up. No recurrence of ulcer was
noticed in both groups. Table 1: Sex distribution
Laparoscopic surgery minimizes postoperative wound Sex Number of cases %
pain, encourages early mobilization and return to normal. Male 49 80
Daily activities. The benet of early discharge and early Female 12 20
return to work may outweigh the consumable cost incurred. Total 61 100
In the execution of the laparoscopic procedures, the role
of laparoscopic surgery in emergencies is well-documented. Table 2: Age distribution
The change of disease pattern in perforated peptic ulcer Age Number of cases %
favors a simple repair procedure. With the demonstrated 21-40 23 37
benet in our trial, laparoscopic repair of perforated peptic 41-60 35 57
61-80 3 4
ulcers should be the procedure of choice. Laparoscopy
should be incorporated into the general surgeon’s Total 61 100
World Journal of Laparoscopic Surgery, January-April 2013;6(1):11-14 13