Page 30 - World Journal of Laparoscopic Surgery
P. 30
Boy Busmar
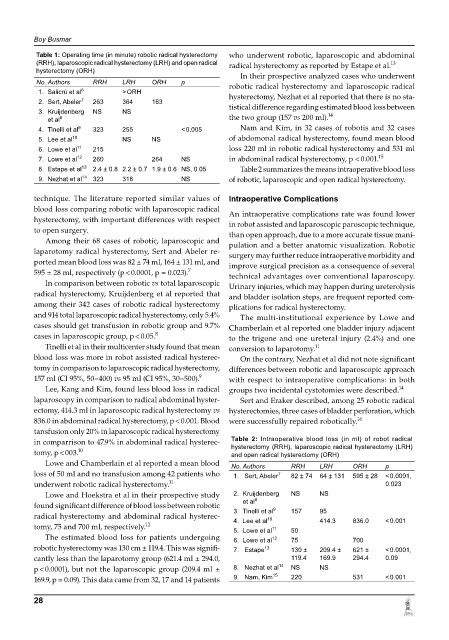
Table 1: Operating time (in minute) robotic radical hysterectomy who underwent robotic, laparoscopic and abdominal
(RRH), laparoscopic radical hysterectomy (LRH) and open radical radical hysterectomy as reported by Estape et al. 13
hysterectomy (ORH)
In their prospective analyzed cases who underwent
No. Authors RRH LRH ORH p robotic radical hysterectomy and laparoscopic radical
6
1. Salicrú et al > oRh hysterectomy, Nezhat et al reported that there is no sta-
2. Sert, Abeler 7 263 364 163
3. Kruijdenberg nS nS tistical difference regarding estimated blood loss between
14
8
et al the two group (157 vs 200 ml).
4. Tinelli et al 9 323 255 < 0.005 Nam and Kim, in 32 cases of robotis and 32 cases
5. lee et al 10 nS nS of abdomonal radical hysterectomy, found mean blood
6. lowe et al 11 215 loss 220 ml in robotic radical hysterectomy and 531 ml
7. lowe et al 12 260 264 nS in abdominal radical hysterectomy, p < 0.001. 15
8. estape et al 13 2.4 ± 0.8 2.2 ± 0.7 1.9 ± 0.6 NS, 0.05 Table 2 summarizes the means intraoperative blood loss
9. nezhat et al 14 323 318 nS of robotic, laparoscopic and open radical hysterectomy.
technique. The literature reported similar values of intraoperative Complications
blood loss comparing robotic with laparoscopic radical An intraoperative complications rate was found lower
hysterectomy, with important differences with respect in robot assisted and laparoscopic paroscopic technique,
to open surgery. than open approach, due to a more accurate tissue mani-
Among their 68 cases of robotic, laparoscopic and pulation and a better anatomic visualization. Robotic
laparotomy radical hysterectomy, Sert and Abeler re- surgery may further reduce intraoperative morbidity and
ported mean blood loss was 82 ± 74 ml, 164 ± 131 ml, and improve surgical precision as a consequence of several
595 ± 28 ml, respectively (p < 0.0001, p = 0.023). 7 technical advantages over conventional laparoscopy.
In comparison between robotic vs total laparoscopic Urinary injuries, which may happen during ureterolysis
radical hysterectomy, Kruijdenberg et al reported that and bladder isolation steps, are frequent reported com-
among their 342 cases of robotic radical hysterectomy plications for radical hysterectomy.
and 914 total laparoscopic radical hysterectomy, only 5.4% The multi-institutional experience by Lowe and
cases should get transfusion in robotic group and 9.7% Chamberlain et al reported one bladder injury adjacent
cases in laparoscopic group, p < 0.05. 8 to the trigone and one ureteral injury (2.4%) and one
Tinelli et al in their multicenter study found that mean conversion to laparotomy. 11
blood loss was more in robot assisted radical hysterec- On the contrary, Nezhat et al did not note significant
tomy in comparison to laparoscopic radical hysterectomy, differences between robotic and laparoscopic approach
157 ml (CI 95%, 50–400) vs 95 ml (CI 95%, 30–500). 9 with respect to intraoperative complications: in both
Lee, Kang and Kim, found less blood loss in radical groups two incidental cystotomies were described. 14
laparoscopy in comparison to radical abdominal hyster- Sert and Eraker described, among 25 robotic radical
ectomy, 414.3 ml in laparoscopic radical hysterectomy vs hysterectomies, three cases of bladder perforation, which
16
836.0 in abdominal radical hysterectomy, p < 0.001. Blood were successfully repaired robotically.
tansfusion only 20% in laparoscopic radical hysterectomy
in comparrison to 47.9% in abdominal radical hysterec- Table 2: Intraoperative blood loss (in ml) of robot radical
hysterectomy (RRH), laparoscopic radical hysterectomy (LRH)
tomy, p < 003. 10 and open radical hysterectomy (ORH)
Lowe and Chamberlain et al reported a mean blood No. Authors RRH LRH ORH p
loss of 50 ml and no transfusion among 42 patients who 1. Sert, Abeler 7 82 ± 74 64 ± 131 595 ± 28 < 0.0001,
underwent robotic radical hysterectomy. 11 0.023
Lowe and Hoekstra et al in their prospective study 2. Kruijdenberg nS nS
8
et al
found significant difference of blood loss between robotic 3. Tinelli et al 9 157 95
radical hysterectomy and abdominal radical hysterec- 4. lee et al 10 414.3 836.0 < 0.001
tomy, 75 and 700 ml, respectively. 12 5. lowe et al 11 50
The estimated blood loss for patients undergoing 6. lowe et al 12 75 700
robotic hysterectomy was 130 cm ± 119.4. This was signifi- 7. estape 13 130 ± 209.4 ± 621 ± < 0.0001,
cantly less than the laparotomy group (621.4 ml ± 294.0, 119.4 169.9 294.4 0.09
p < 0.0001), but not the laparoscopic group (209.4 ml ± 8. nezhat et al 14 nS nS
169.9, p = 0.09). This data came from 32, 17 and 14 patients 9. Nam, Kim 15 220 531 < 0.001
28