Page 47 - World Journal of Laparoscopic Surgery
P. 47
WJOLS
Early Postoperative Small Bowel Obstruction associated with the use of V-loc Sutures during Surgery for POP
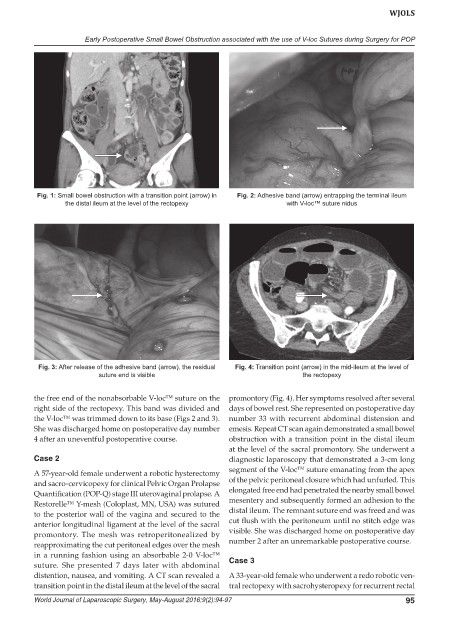
Fig. 1: Small bowel obstruction with a transition point (arrow) in Fig. 2: Adhesive band (arrow) entrapping the terminal ileum
the distal ileum at the level of the rectopexy with V-loc™ suture nidus
Fig. 3: After release of the adhesive band (arrow), the residual Fig. 4: Transition point (arrow) in the mid-ileum at the level of
suture end is visible the rectopexy
the free end of the nonabsorbable V-loc™ suture on the promontory (Fig. 4). Her symptoms resolved after several
right side of the rectopexy. This band was divided and days of bowel rest. She represented on postoperative day
the V-loc™ was trimmed down to its base (Figs 2 and 3). number 33 with recurrent abdominal distension and
She was discharged home on postoperative day number emesis. Repeat CT scan again demonstrated a small bowel
4 after an uneventful postoperative course. obstruction with a transition point in the distal ileum
at the level of the sacral promontory. She underwent a
Case 2 diagnostic laparoscopy that demonstrated a 3-cm long
segment of the V-loc™ suture emanating from the apex
A 57-year-old female underwent a robotic hysterectomy
and sacro-cervicopexy for clinical Pelvic Organ Prolapse of the pelvic peritoneal closure which had unfurled. This
Quantification (POP-Q) stage III uterovaginal prolapse. A elongated free end had penetrated the nearby small bowel
Restorelle™ Y-mesh (Coloplast, MN, USA) was sutured mesentery and subsequently formed an adhesion to the
to the posterior wall of the vagina and secured to the distal ileum. The remnant suture end was freed and was
anterior longitudinal ligament at the level of the sacral cut flush with the peritoneum until no stitch edge was
promontory. The mesh was retroperitonealized by visible. She was discharged home on postoperative day
reapproximating the cut peritoneal edges over the mesh number 2 after an unremarkable postoperative course.
in a running fashion using an absorbable 2-0 V-loc™
suture. She presented 7 days later with abdominal Case 3
distention, nausea, and vomiting. A CT scan revealed a A 33-year-old female who underwent a redo robotic ven-
transition point in the distal ileum at the level of the sacral tral rectopexy with sacrohysteropexy for recurrent rectal
World Journal of Laparoscopic Surgery, May-August 2016;9(2):94-97 95