Page 28 - World Journal of Laparoscopic Surgery
P. 28
BV Sharath
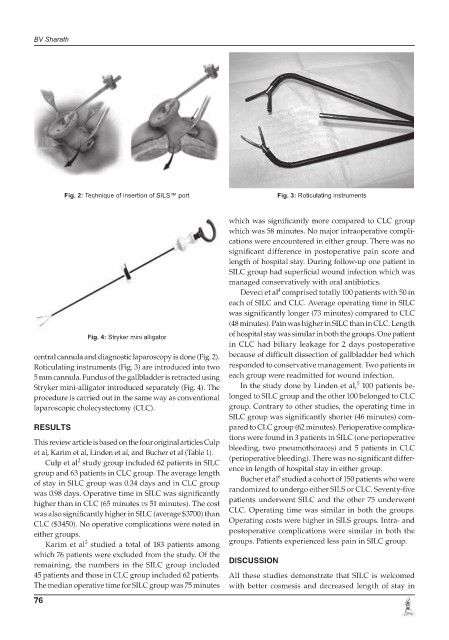
Fig. 2: Technique of insertion of SILS™ port Fig. 3: Roticulating instruments
which was significantly more compared to CLC group
which was 58 minutes. No major intraoperative compli-
cations were encountered in either group. There was no
significant difference in postoperative pain score and
length of hospital stay. During follow-up one patient in
SILC group had superficial wound infection which was
managed conservatively with oral antibiotics.
4
Deveci et al comprised totally 100 patients with 50 in
each of SILC and CLC. Average operating time in SILC
was significantly longer (73 minutes) compared to CLC
(48 minutes). Pain was higher in SILC than in CLC. Length
Fig. 4: Stryker mini alligator of hospital stay was similar in both the groups. One patient
in CLC had biliary leakage for 2 days postoperative
central cannula and diagnostic laparoscopy is done (Fig. 2). because of difficult dissection of gallbladder bed which
Roticulating instruments (Fig. 3) are introduced into two responded to conservative management. Two patients in
5 mm cannula. Fundus of the gallbladder is retracted using each group were readmitted for wound infection.
5
Stryker mini-alligator introduced separately (Fig. 4). The In the study done by Linden et al, 100 patients be-
procedure is carried out in the same way as conventional longed to SILC group and the other 100 belonged to CLC
laparoscopic cholecystectomy (CLC). group. Contrary to other studies, the operating time in
SILC group was significantly shorter (46 minutes) com-
RESULTS pared to CLC group (62 minutes). Perioperative complica-
tions were found in 3 patients in SILC (one perioperative
This review article is based on the four original articles Culp
et al, Karim et al, Linden et al, and Bucher et al (Table 1). bleeding, two pneumothoraces) and 5 patients in CLC
2
Culp et al study group included 62 patients in SILC (perioperative bleeding). There was no significant differ-
group and 63 patients in CLC group. The average length ence in length of hospital stay in either group.
6
of stay in SILC group was 0.34 days and in CLC group Bucher et al studied a cohort of 150 patients who were
was 0.98 days. Operative time in SILC was significantly randomized to undergo either SILS or CLC. Seventy-five
higher than in CLC (65 minutes vs 51 minutes). The cost patients underwent SILC and the other 75 underwent
was also significantly higher in SILC (average $3700) than CLC. Operating time was similar in both the groups.
CLC ($3450). No operative complications were noted in Operating costs were higher in SILS groups. Intra- and
either groups. postoperative complications were similar in both the
3
Karim et al studied a total of 183 patients among groups. Patients experienced less pain in SILC group.
which 76 patients were excluded from the study. Of the
remaining, the numbers in the SILC group included DISCUSSION
45 patients and those in CLC group included 62 patients. All these studies demonstrate that SILC is welcomed
The median operative time for SILC group was 75 minutes with better cosmesis and decreased length of stay in
76