Page 5 - World Journal of Laparoscopic Surgery
P. 5
WJOLS
Laparoscopic Sleeve Gastrectomy—A Novel Surgical Tool for Weight Loss in morbidly Obese Patients
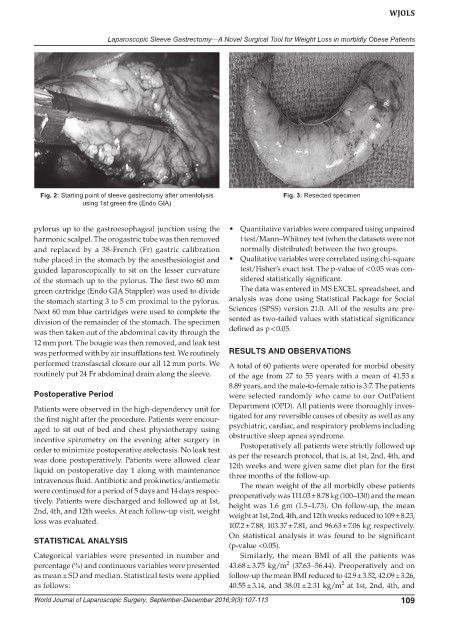
Fig. 2: Starting point of sleeve gastrectomy after omentolysis Fig. 3: Resected specimen
using 1st green fire (Endo GIA)
pylorus up to the gastroesophageal junction using the • Quantitative variables were compared using unpaired
harmonic scalpel. The orogastric tube was then removed t test/Mann–Whitney test (when the datasets were not
and replaced by a 38-French (Fr) gastric calibration normally distributed) between the two groups.
tube placed in the stomach by the anesthesiologist and • Qualitative variables were correlated using chi-square
guided laparoscopically to sit on the lesser curvature test/Fisher’s exact test. The p-value of < 0.05 was con-
of the stomach up to the pylorus. The first two 60 mm sidered statistically significant.
green cartridge (Endo GIA Stappler) was used to divide The data was entered in MS EXCEL spreadsheet, and
the stomach starting 3 to 5 cm proximal to the pylorus. analysis was done using Statistical Package for Social
Next 60 mm blue cartridges were used to complete the Sciences (SPSS) version 21.0. All of the results are pre-
division of the remainder of the stomach. The specimen sented as two-tailed values with statistical significance
was then taken out of the abdominal cavity through the defined as p < 0.05.
12 mm port. The bougie was then removed, and leak test
was performed with by air insufflations test. We routinely RESULTS AND OBSERVATIONS
performed transfascial closure our all 12 mm ports. We A total of 60 patients were operated for morbid obesity
routinely put 24 Fr abdominal drain along the sleeve. of the age from 27 to 55 years with a mean of 41.53 ±
8.89 years, and the male-to-female ratio is 3:7. The patients
Postoperative Period were selected randomly who came to our OutPatient
Patients were observed in the high-dependency unit for Department (OPD). All patients were thoroughly inves-
the first night after the procedure. Patients were encour- tigated for any reversible causes of obesity as well as any
aged to sit out of bed and chest physiotherapy using psychiatric, cardiac, and respiratory problems including
incentive spirometry on the evening after surgery in obstructive sleep apnea syndrome.
order to minimize postoperative atelectasis. No leak test Postoperatively all patients were strictly followed up
was done postoperatively. Patients were allowed clear as per the research protocol, that is, at 1st, 2nd, 4th, and
liquid on postoperative day 1 along with maintenance 12th weeks and were given same diet plan for the first
intravenous fluid. Antibiotic and prokinetics/antiemetic three months of the follow-up.
The mean weight of the all morbidly obese patients
were continued for a period of 5 days and 14 days respec- preoperatively was 111.03 ± 8.78 kg (100–130) and the mean
tively. Patients were discharged and followed up at 1st, height was 1.6 gm (1.5–1.73). On follow-up, the mean
2nd, 4th, and 12th weeks. At each follow-up visit, weight weight at 1st, 2nd, 4th, and 12th weeks reduced to 109 ± 8.23,
loss was evaluated.
107.2 ± 7.88, 103.37 ± 7.81, and 96.63 ± 7.06 kg respectively.
On statistical analysis it was found to be significant
STATISTICAL ANALYSIS
(p-value <0.05).
Categorical variables were presented in number and Similarly, the mean BMI of all the patients was
2
percentage (%) and continuous variables were presented 43.68 ± 3.75 kg/m (37.63–56.44). Preoperatively and on
as mean ± SD and median. Statistical tests were applied follow-up the mean BMI reduced to 42.9 ± 3.52, 42.09 ± 3.26,
2
as follows: 40.55 ± 3.14, and 38.01 ± 2.31 kg/m at 1st, 2nd, 4th, and
World Journal of Laparoscopic Surgery, September-December 2016;9(3):107-113 109