Page 19 - World Journal of Laparoscopic Surgery
P. 19
WJOLS
Challenges in the Widespread Use of Minimal Access Surgery for the Management of Abdominal Trauma: A Primer
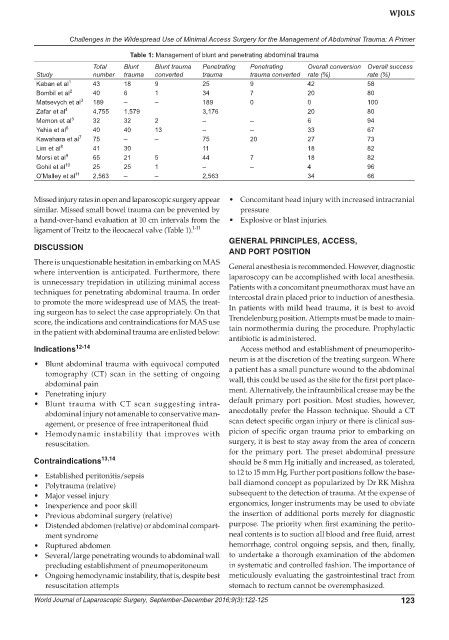
Table 1: Management of blunt and penetrating abdominal trauma
Total Blunt Blunt trauma Penetrating Penetrating Overall conversion Overall success
Study number trauma converted trauma trauma converted rate (%) rate (%)
Kaban et al 1 43 18 9 25 9 42 58
Bombil et al 2 40 6 1 34 7 20 80
Matsevych et al 3 189 – – 189 0 0 100
Zafar et al 4 4,755 1,579 3,176 20 80
Memon et al 5 32 32 2 – – 6 94
Yehia et al 6 40 40 13 – – 33 67
Kawahara et al 7 75 – – 75 20 27 73
Lim et al 8 41 30 11 18 82
Morsi et al 9 65 21 5 44 7 18 82
Gohil et al 10 25 25 1 – – 4 96
O’Malley et al 11 2,563 – – 2,563 34 66
Missed injury rates in open and laparoscopic surgery appear • Concomitant head injury with increased intracranial
similar. Missed small bowel trauma can be prevented by pressure
a hand-over-hand evaluation at 10 cm intervals from the • Explosive or blast injuries.
ligament of Treitz to the ileocaecal valve (Table 1). 1-11
GENERAL PRINCIPLES, ACCESS,
DISCUSSION
AND PORT POSITION
There is unquestionable hesitation in embarking on MAS General anesthesia is recommended. However, diagnostic
where intervention is anticipated. Furthermore, there laparoscopy can be accomplished with local anesthesia.
is unnecessary trepidation in utilizing minimal access
techniques for penetrating abdominal trauma. In order Patients with a concomitant pneumothorax must have an
to promote the more widespread use of MAS, the treat- intercostal drain placed prior to induction of anesthesia.
ing surgeon has to select the case appropriately. On that In patients with mild head trauma, it is best to avoid
score, the indications and contraindications for MAS use Trendelenburg position. Attempts must be made to main-
in the patient with abdominal trauma are enlisted below: tain normothermia during the procedure. Prophylactic
antibiotic is administered.
Indications 12-14 Access method and establishment of pneumoperito-
neum is at the discretion of the treating surgeon. Where
• Blunt abdominal trauma with equivocal computed
tomography (CT) scan in the setting of ongoing a patient has a small puncture wound to the abdominal
abdominal pain wall, this could be used as the site for the first port place-
• Penetrating injury ment. Alternatively, the infraumbilical crease may be the
• Blunt trauma with CT scan suggesting intra- default primary port position. Most studies, however,
abdominal injury not amenable to conservative man- anecdotally prefer the Hasson technique. Should a CT
agement, or presence of free intraperitoneal fluid scan detect specific organ injury or there is clinical sus-
• Hemodynamic instability that improves with picion of specific organ trauma prior to embarking on
resuscitation. surgery, it is best to stay away from the area of concern
for the primary port. The preset abdominal pressure
Contraindications 13,14 should be 8 mm Hg initially and increased, as tolerated,
• Established peritonitis/sepsis to 12 to 15 mm Hg. Further port positions follow the base-
• Polytrauma (relative) ball diamond concept as popularized by Dr RK Mishra
• Major vessel injury subsequent to the detection of trauma. At the expense of
• Inexperience and poor skill ergonomics, longer instruments may be used to obviate
• Previous abdominal surgery (relative) the insertion of additional ports merely for diagnostic
• Distended abdomen (relative) or abdominal compart- purpose. The priority when first examining the perito-
ment syndrome neal contents is to suction all blood and free fluid, arrest
• Ruptured abdomen hemorrhage, control ongoing sepsis, and then, finally,
• Several/large penetrating wounds to abdominal wall to undertake a thorough examination of the abdomen
precluding establishment of pneumoperitoneum in systematic and controlled fashion. The importance of
• Ongoing hemodynamic instability, that is, despite best meticulously evaluating the gastrointestinal tract from
resuscitation attempts stomach to rectum cannot be overemphasized.
World Journal of Laparoscopic Surgery, September-December 2016;9(3):122-125 123