Page 12 - World Journal of Laparoscopic Surgery
P. 12
Garima Gupta et al
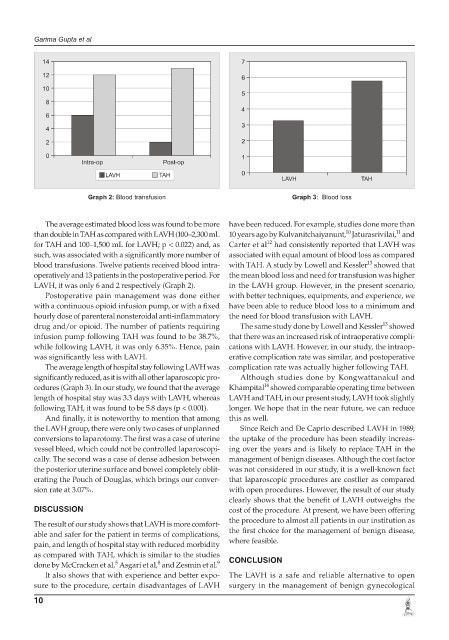
Graph 2: Blood transfusion Graph 3: Blood loss
The average estimated blood loss was found to be more have been reduced. For example, studies done more than
10
11
than double in TAH as compared with LAVH (100–2,300 mL 10 years ago by Kulvanitchaiyanunt, Jaturasrivilai, and
12
for TAH and 100–1,500 mL for LAVH; p < 0.022) and, as Carter et al had consistently reported that LAVH was
such, was associated with a significantly more number of associated with equal amount of blood loss as compared
13
blood transfusions. Twelve patients received blood intra- with TAH. A study by Lowell and Kessler showed that
operatively and 13 patients in the postoperative period. For the mean blood loss and need for transfusion was higher
LAVH, it was only 6 and 2 respectively (Graph 2). in the LAVH group. However, in the present scenario,
Postoperative pain management was done either with better techniques, equipments, and experience, we
with a continuous opioid infusion pump, or with a fixed have been able to reduce blood loss to a minimum and
hourly dose of parenteral nonsteroidal anti-inflammatory the need for blood transfusion with LAVH.
13
drug and/or opioid. The number of patients requiring The same study done by Lowell and Kessler showed
infusion pump following TAH was found to be 38.7%, that there was an increased risk of intraoperative compli-
while following LAVH, it was only 6.35%. Hence, pain cations with LAVH. However, in our study, the intraop-
was significantly less with LAVH. erative complication rate was similar, and postoperative
The average length of hospital stay following LAVH was complication rate was actually higher following TAH.
significantly reduced, as it is with all other laparoscopic pro- Although studies done by Kongwattanakul and
14
cedures (Graph 3). In our study, we found that the average Khampital showed comparable operating time between
length of hospital stay was 3.3 days with LAVH, whereas LAVH and TAH, in our present study, LAVH took slightly
following TAH, it was found to be 5.8 days (p < 0.001). longer. We hope that in the near future, we can reduce
And finally, it is noteworthy to mention that among this as well.
the LAVH group, there were only two cases of unplanned Since Reich and De Caprio described LAVH in 1989,
conversions to laparotomy. The first was a case of uterine the uptake of the procedure has been steadily increas-
vessel bleed, which could not be controlled laparoscopi- ing over the years and is likely to replace TAH in the
cally. The second was a case of dense adhesion between management of benign diseases. Although the cost factor
the posterior uterine surface and bowel completely oblit- was not considered in our study, it is a well-known fact
erating the Pouch of Douglas, which brings our conver- that laparoscopic procedures are costlier as compared
sion rate at 3.07%. with open procedures. However, the result of our study
clearly shows that the benefit of LAVH outweighs the
DISCUSSION cost of the procedure. At present, we have been offering
the procedure to almost all patients in our institution as
The result of our study shows that LAVH is more comfort-
able and safer for the patient in terms of complications, the first choice for the management of benign disease,
pain, and length of hospital stay with reduced morbidity where feasible.
as compared with TAH, which is similar to the studies
8
5
done by McCracken et al, Asgari et al, and Zesmin et al. 9 CONCLUSION
It also shows that with experience and better expo- The LAVH is a safe and reliable alternative to open
sure to the procedure, certain disadvantages of LAVH surgery in the management of benign gynecological
10