Page 30 - Journal of World Association of Laparoscopic Surgeons
P. 30
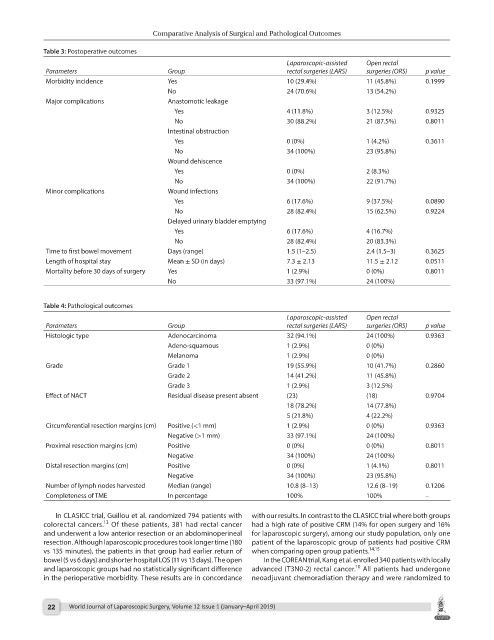
Comparative Analysis of Surgical and Pathological Outcomes
Table 3: Postoperative outcomes
Laparoscopic-assisted Open rectal
Parameters Group rectal surgeries (LARS) surgeries (ORS) p value
Morbidity incidence Yes 10 (29.4%) 11 (45.8%) 0.1999
No 24 (70.6%) 13 (54.2%)
Major complications Anastomotic leakage
Yes 4 (11.8%) 3 (12.5%) 0.9325
No 30 (88.2%) 21 (87.5%) 0.8011
Intestinal obstruction
Yes 0 (0%) 1 (4.2%) 0.3611
No 34 (100%) 23 (95.8%)
Wound dehiscence
Yes 0 (0%) 2 (8.3%)
No 34 (100%) 22 (91.7%)
Minor complications Wound infections
Yes 6 (17.6%) 9 (37.5%) 0.0890
No 28 (82.4%) 15 (62.5%) 0.9224
Delayed urinary bladder emptying
Yes 6 (17.6%) 4 (16.7%)
No 28 (82.4%) 20 (83.3%)
Time to first bowel movement Days (range) 1.5 (1–2.5) 2.4 (1.5–3) 0.3625
Length of hospital stay Mean ± SD (in days) 7.3 ± 2.13 11.5 ± 2.12 0.0511
Mortality before 30 days of surgery Yes 1 (2.9%) 0 (0%) 0.8011
No 33 (97.1%) 24 (100%)
Table 4: Pathological outcomes
Laparoscopic-assisted Open rectal
Parameters Group rectal surgeries (LARS) surgeries (ORS) p value
Histologic type Adenocarcinoma 32 (94.1%) 24 (100%) 0.9363
Adeno-squamous 1 (2.9%) 0 (0%)
Melanoma 1 (2.9%) 0 (0%)
Grade Grade 1 19 (55.9%) 10 (41.7%) 0.2860
Grade 2 14 (41.2%) 11 (45.8%)
Grade 3 1 (2.9%) 3 (12.5%)
Effect of NACT Residual disease present absent (23) (18) 0.9704
18 (78.2%) 14 (77.8%)
5 (21.8%) 4 (22.2%)
Circumferential resection margins (cm) Positive (<1 mm) 1 (2.9%) 0 (0%) 0.9363
Negative (>1 mm) 33 (97.1%) 24 (100%)
Proximal resection margins (cm) Positive 0 (0%) 0 (0%) 0.8011
Negative 34 (100%) 24 (100%)
Distal resection margins (cm) Positive 0 (0%) 1 (4.1%) 0.8011
Negative 34 (100%) 23 (95.8%)
Number of lymph nodes harvested Median (range) 10.8 (8–13) 12.6 (8–19) 0.1206
Completeness of TME In percentage 100% 100% –
In CLASICC trial, Guillou et al. randomized 794 patients with with our results. In contrast to the CLASICC trial where both groups
13
colorectal cancers. Of these patients, 381 had rectal cancer had a high rate of positive CRM (14% for open surgery and 16%
and underwent a low anterior resection or an abdominoperineal for laparoscopic surgery), among our study population, only one
resection. Although laparoscopic procedures took longer time (180 patient of the laparoscopic group of patients had positive CRM
14,15
vs 135 minutes), the patients in that group had earlier return of when comparing open group patients.
bowel (5 vs 6 days) and shorter hospital LOS (11 vs 13 days). The open In the COREAN trial, Kang et al. enrolled 340 patients with locally
10
and laparoscopic groups had no statistically significant difference advanced (T3N0-2) rectal cancer. All patients had undergone
in the perioperative morbidity. These results are in concordance neoadjuvant chemoradiation therapy and were randomized to
22 World Journal of Laparoscopic Surgery, Volume 12 Issue 1 (January–April 2019)