Page 32 - World Journal of Laparoscopic Surgery
P. 32
Retrocaval Ureter
Table 1: Demographic profile and procedure
Patient Age/ Obstructed drainage Location of
No. sex (Yes/No) stone and size Symptoms Procedure
1 35/M Yes Superior calyx Flank pain Laparoscopic transperitoneal
1.3 × 1.4 cm pyeloureterostomy with rigid nephroscopy
2 45/M Yes Superior calyx Flank pain Laparoscopic transperitoneal
1.6 × 1.5 cm pyeloureterostomy with rigid nephroscopy
3 19/F Yes Inferior calyx Flank pain, Laparoscopic transperitoneal
1.2 × 1.1 cm dysuria, fever pyeloureterostomy with flexible
nephroscopy + laser lithotripsy
4 26/F Yes Pelvis Flank pain Laparoscopic transperitoneal
1.9 × 1.8 cm pyeloureterostomy with rigid nephroscopy
5 33/M Yes Inferior calyx Flank pain, PCNL followed by laparoscopic
2.2 × 1.9 cm dysuria transperitoneal pyeloureterostomy
(same sitting)
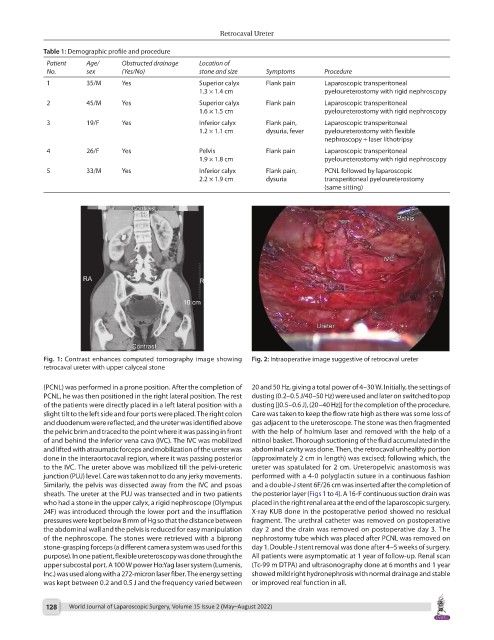
Fig. 1: Contrast enhances computed tomography image showing Fig. 2: Intraoperative image suggestive of retrocaval ureter
retrocaval ureter with upper calyceal stone
(PCNL) was performed in a prone position. After the completion of 20 and 50 Hz, giving a total power of 4–30 W. Initially, the settings of
PCNL, he was then positioned in the right lateral position. The rest dusting (0.2–0.5 J/40–50 Hz) were used and later on switched to pop
of the patients were directly placed in a left lateral position with a dusting [(0.5–0.6 J), (20–40 Hz)] for the completion of the procedure.
slight tilt to the left side and four ports were placed. The right colon Care was taken to keep the flow rate high as there was some loss of
and duodenum were reflected, and the ureter was identified above gas adjacent to the ureteroscope. The stone was then fragmented
the pelvic brim and traced to the point where it was passing in front with the help of holmium laser and removed with the help of a
of and behind the inferior vena cava (IVC). The IVC was mobilized nitinol basket. Thorough suctioning of the fluid accumulated in the
and lifted with atraumatic forceps and mobilization of the ureter was abdominal cavity was done. Then, the retrocaval unhealthy portion
done in the interaortocaval region, where it was passing posterior (approximately 2 cm in length) was excised; following which, the
to the IVC. The ureter above was mobilized till the pelvi-ureteric ureter was spatulated for 2 cm. Ureteropelvic anastomosis was
junction (PUJ) level. Care was taken not to do any jerky movements. performed with a 4-0 polyglactin suture in a continuous fashion
Similarly, the pelvis was dissected away from the IVC and psoas and a double-J stent 6F/26 cm was inserted after the completion of
sheath. The ureter at the PUJ was transected and in two patients the posterior layer (Figs 1 to 4). A 16-F continuous suction drain was
who had a stone in the upper calyx, a rigid nephroscope (Olympus placed in the right renal area at the end of the laparoscopic surgery.
24F) was introduced through the lower port and the insufflation X-ray KUB done in the postoperative period showed no residual
pressures were kept below 8 mm of Hg so that the distance between fragment. The urethral catheter was removed on postoperative
the abdominal wall and the pelvis is reduced for easy manipulation day 2 and the drain was removed on postoperative day 3. The
of the nephroscope. The stones were retrieved with a biprong nephrostomy tube which was placed after PCNL was removed on
stone-grasping forceps (a different camera system was used for this day 1. Double-J stent removal was done after 4–5 weeks of surgery.
purpose). In one patient, flexible ureteroscopy was done through the All patients were asymptomatic at 1 year of follow-up. Renal scan
upper subcostal port. A 100 W power Ho:Yag laser system (Lumenis, (Tc-99 m DTPA) and ultrasonography done at 6 months and 1 year
Inc.) was used along with a 272-micron laser fiber. The energy setting showed mild right hydronephrosis with normal drainage and stable
was kept between 0.2 and 0.5 J and the frequency varied between or improved real function in all.
128 World Journal of Laparoscopic Surgery, Volume 15 Issue 2 (May–August 2022)