Page 46 - Jourmal of World Association of Laparoscopic Surgeon
P. 46
Medhat M Ibrahim
the parents. All the patients received one dose of antibiotic The patient position and the pneumoperitoneal pressure
prophylaxis in the form of ceftriaxone 50 mg/kg at the time often aids in the reduction of the hernial content to the
of induction of anesthesia. All patients went preoperative abdomen and also increase the abdominal cavity space. Once
assessment aiming to exclude patients with significant the intestine was reduced into the abdomen, the falciform
pulmonary hyperplasia and identify other congenital ligament of the liver was dissected by the harmonic dissector
anomalies. Preoxygenation with O 100% without positive to free the liver from the diaphragm and also remove all the
2
pressure was done. The routine monitoring as pulse tissue passing from the abdomen to the chest though the
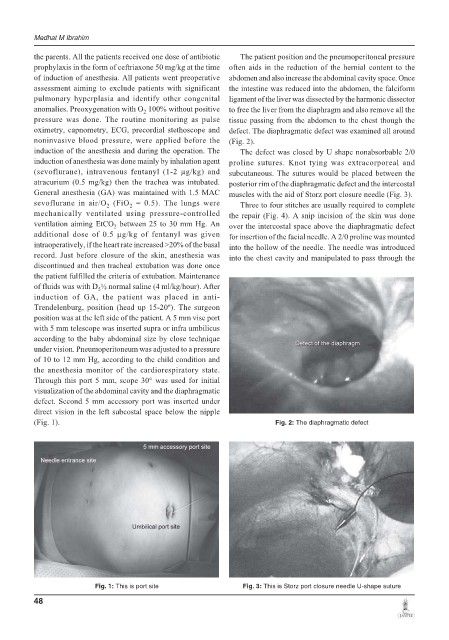
oximetry, capnometry, ECG, precordial stethoscope and defect. The diaphragmatic defect was examined all around
noninvasive blood pressure, were applied before the (Fig. 2).
induction of the anesthesia and during the operation. The The defect was closed by U shape nonabsorbable 2/0
induction of anesthesia was done mainly by inhalation agent proline sutures. Knot tying was extracorporeal and
(sevoflurane), intravenous fentanyl (1-2 μg/kg) and subcutaneous. The sutures would be placed between the
atracurium (0.5 mg/kg) then the trachea was intubated. posterior rim of the diaphragmatic defect and the intercostal
General anesthesia (GA) was maintained with 1.5 MAC muscles with the aid of Storz port closure needle (Fig. 3).
sevoflurane in air/O (FiO = 0.5). The lungs were Three to four stitches are usually required to complete
2
2
mechanically ventilated using pressure-controlled the repair (Fig. 4). A snip incision of the skin was done
ventilation aiming EtCO between 25 to 30 mm Hg. An over the intercostal space above the diaphragmatic defect
2
additional dose of 0.5 μg/kg of fentanyl was given for insertion of the facial needle. A 2/0 proline was mounted
intraoperatively, if the heart rate increased >20% of the basal into the hollow of the needle. The needle was introduced
record. Just before closure of the skin, anesthesia was into the chest cavity and manipulated to pass through the
discontinued and then tracheal extubation was done once
the patient fulfilled the criteria of extubation. Maintenance
of fluids was with D ½ normal saline (4 ml/kg/hour). After
5
induction of GA, the patient was placed in anti-
Trendelenburg, position (head up 15-20º). The surgeon
position was at the left side of the patient. A 5 mm vise port
with 5 mm telescope was inserted supra or infra umbilicus
according to the baby abdominal size by close technique
under vision. Pneumoperitoneum was adjusted to a pressure
of 10 to 12 mm Hg, according to the child condition and
the anesthesia monitor of the cardiorespiratory state.
Through this port 5 mm, scope 30° was used for initial
visualization of the abdominal cavity and the diaphragmatic
defect. Second 5 mm accessory port was inserted under
direct vision in the left subcostal space below the nipple
(Fig. 1). Fig. 2: The diaphragmatic defect
Fig. 1: This is port site Fig. 3: This is Storz port closure needle U-shape suture
48