Page 37 - Jourmal of World Association of Laparoscopic Surgeon
P. 37
WJOLS
Is Minimal Access Surgery of Esophageal Atresia with Distal Esophageal Atresia by Thoracoscopy is
14
Table 2: Comparison with open thoracotomy with recent studies related. The mortality by Tariq et al was 3, Pakowaski
16
done by Burford and historical study as control et al was 3, Van der Zee et al was 2 but none of them is
21
Burford serried 4 Historic control 5-8 found due to surgical related.
18
4
No. of patient 72 340 Holocomb et al and Burford et al mentioned scoliosis
Anastomotic leak 2.7% 17.9% and higher right shoulder deformity in OR group. None of
Stricture 5.50% 16.7%
Recurrent fistula 2.70% 7.9% the literature mentioned such complication in TR group.
Fundoplication 12.50% 21%
DISCUSSION
Postoperative stricture formation is another squella of
4
ES/TEF surgery. Holocomb et al found a significant Advancement in the minimal access surgery have been used
in adult for long time but later on it has been used
difference with lower rate in TR vs OR group (7.6% vs 22
17.9% respectively) (Fig. 2). increasingly in pediatric surgery. This evolution lead the
Gastroesophageal reflux is common after EA with TEF surgeon to address the most of the congenital anomalies by
repair and needs to address. Nowadays all cases are treated minimal access surgery and several report have revealed
23
medically however, a number of patients need antireflux the safety in pediatric patients. Initially it was hypothesized
4
surgery. 19,20 Holocomb et al showed that 24% of that neonate may not be able to tolerate the burden of CO 2
12
thoracoscopy patient need fundoplication. The historical but comparative studies done by Ma Li et al showed same
5-8
data showed fundoplication rate from 15 to 45%. Burford ET CO in TR and OR groups without any significant
2
4
et al in his study of open thoracotomy mentioned 12.5% difference (Fig. 3). Although pCO increased intra-
2
patient need fundoplication. operatively but reduced at the end of surgery. Similar studies
24
There is no difference in the incidence of recurrent fistula were done by Matsunari with the finding that thoracoscopy
in either group and incidence is between 0 and 5%. group had a higher incidence of intraoperative hypercapnia
Few literature mentioned death but it is difficult to and acidosis and required higher inspired oxygen fraction
ascertain that whether it is pure surgical related or medical but on admission to ICU Pa(CO ) was in the normal range
2
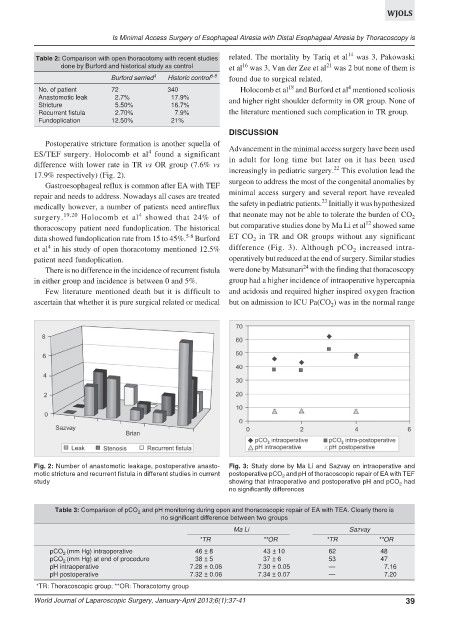
Fig. 2: Number of anastomotic leakage, postoperative anasto- Fig. 3: Study done by Ma Li and Sazvay on intraoperative and
motic stricture and recurrent fistula in different studies in current postoperative pCO and pH of thoracoscopic repair of EA with TEF
2
study showing that intraoperative and postoperative pH and pCO had
2
no significantly differences
Table 3: Comparison of pCO and pH monitoring during open and thoracoscopic repair of EA with TEA. Clearly there is
2
no significant difference between two groups
Ma Li Sazvay
*TR **OR *TR **OR
pCO (mm Hg) intraoperative 46 ± 8 43 ± 10 62 48
2
pCO (mm Hg) at end of procedure 38 ± 5 37 ± 6 53 47
2
pH intraoperative 7.28 ± 0.06 7.30 ± 0.05 — 7.16
pH postoperative 7.32 ± 0.06 7.34 ± 0.07 — 7.20
*TR: Thoracoscopic group; **OR: Thoracotomy group
World Journal of Laparoscopic Surgery, January-April 2013;6(1):37-41 39