Page 36 - Jourmal of World Association of Laparoscopic Surgeon
P. 36
Usman Javaid
due to number of patients and have control study either with between thoracoscopic and open thoracotomy group (179
open thoracotomy or historical review. There were some and 123 minutes and 149 and 156 minutes respectively).
16
individual papers which mentioned only the outcome of Patkowski reported higher time initially but significant
minimal access surgery by thoracoscopy without control improvement after gaining experience (mean 171 minutes
study. 9,10 Similarly, some studies have small number of for first 10 cases reduce to mean 98 minutes for last
11
patient also which were not included. These data were 13 cases).
collected from the literature and compared with the open Neonatal tolerance to pneumothorax with CO showed
2
thoracotomy approach based on text book and some recent hypercarbia 1 hour after the surgery in both groups, although
literature (Table 1). ET CO was higher in TR group but not reached to
2
The review of literature showed no difference of minimal significant difference (Table 3). 12
access (MAS) surgery between thoracoscopy (TR group) In other study the impact of CO also showed almost
2
17
and open thoracotomy (OR group) in EA with TEF in regard same result by Mark Bishay however in their study
of gestational age of patient, with average age of 2.7 to although the pH became normal at the end of surgery but
3.5 days. Similarly, associated anomalies were almost same the cerebral oxygen saturation decreased.
13
Szavay in their studies found a significant difference
in both groups. Both groups operated premature babies of pCO max in both groups with higher level in TR group
2
successfully. (62 vs 48 respectively; p = 0.014) (Table 3).
13
12
Ma Li and Sazavay revealed a significant difference Perioperative surgical complications were also
in operation time between TR and OR groups (185 vs 148 mentioned in the literature including two tracheal injuries
14
and open 106 vs 141 minutes), but Tariq et al and Brian in TR group. No other perioperative complication is
15
Lugo did not find significant difference in operation time 16
mentioned in the literature other than that in both groups.
Postoperative ventilation and pain has been studied also
but most of literature did not reach to significant difference.
15
However Brian Lugo found significant difference in TR
and OR group in regard of postoperative ventilation (4.6 vs
19 days) and need of narcotics analgesia (5 vs 23.1 days).
14
Tariq et al reported early postoperative complication
which significantly happened in OR group with lung
collapse, pneumonia, chylothorax, recurrent laryngeal nerve
injury and wound infection.
4
18
Holocomb et al and Burfurd et al found longer hospital
stay in OR group as compared to TR group (29 vs 18.1 days
14
and 66 vs 21 days respectively). Tariq et al found no
difference in hospital stay.
The rate of anastomotic leak in either group in all
literature did not reach to significant level and none of leak
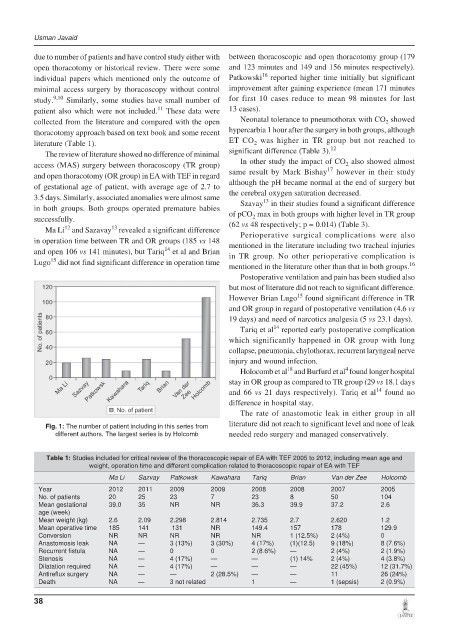
Fig. 1: The number of patient including in this series from
different authors. The largest series is by Holcomb needed redo surgery and managed conservatively.
Table 1: Studies included for critical review of the thoracoscopic repair of EA with TEF 2005 to 2012, including mean age and
weight, operation time and different complication related to thoracoscopic repair of EA with TEF
Ma Li Sazvay Patkowsk Kawahara Tariq Brian Van der Zee Holcomb
Year 2012 2011 2009 2009 2008 2008 2007 2005
No. of patients 20 25 23 7 23 8 50 104
Mean gestational 39.0 35 NR NR 36.3 39.9 37.2 2.6
age (week)
Mean weight (kg) 2.6 2.09 2.298 2.814 2.735 2.7 2.620 1.2
Mean operative time 185 141 131 NR 149.4 157 178 129.9
Conversion NR NR NR NR NR 1 (12.5%) 2 (4%) 0
Anastomosis leak NA — 3 (13%) 3 (30%) 4 (17%) (1)(12.5) 9 (18%) 8 (7.6%)
Recurrent fistula NA — 0 0 2 (8.6%) — 2 (4%) 2 (1.9%)
Stenosis NA — 4 (17%) — — (1) 14% 2 (4%) 4 (3.8%)
Dilatation required NA — 4 (17%) — — — 22 (45%) 12 (31.7%)
Antireflux surgery NA — — 2 (28.5%) — — 11 26 (24%)
Death NA — 3 not related 1 — 1 (sepsis) 2 (0.9%)
38