Page 5 - World Journal of Laparoscopic Surgery
P. 5
WJOLS
Comparison of Open and Laparoscopic Radical Cystectomy for Bladder Cancer: Safety and Early Oncological Results
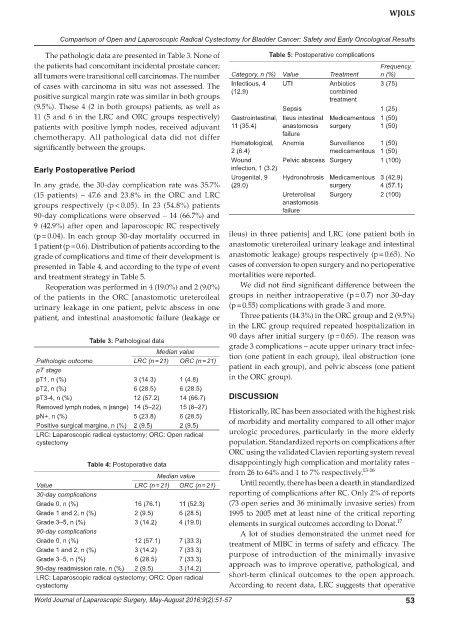
The pathologic data are presented in Table 3. None of Table 5: Postoperative complications
the patients had concomitant incidental prostate cancer; Frequency,
all tumors were transitional cell carcinomas. The number Category, n (%) Value Treatment n (%)
of cases with carcinoma in situ was not assessed. The Infectious, 4 UTI Anbiotics 3 (75)
(12.9)
combined
positive surgical margin rate was similar in both groups treatment
(9.5%). These 4 (2 in both groups) patients, as well as Sepsis 1 (25)
11 (5 and 6 in the LRC and ORC groups respectively) Gastrointestinal, Ileus intestinal Medicamentous 1 (50)
patients with positive lymph nodes, received adjuvant 11 (35.4) anastomosis surgery 1 (50)
chemotherapy. All pathological data did not differ failure
significantly between the groups. Hematological, Anemia Surveillance 1 (50)
medicamentous 1 (50)
2 (6.4)
Wound Pelvic abscess Surgery 1 (100)
Early Postoperative Period infection, 1 (3.2)
Urogenital, 9 Hydronohrosis Medicamentous 3 (42.9)
In any grade, the 30-day complication rate was 35.7% (29.0) surgery 4 (57.1)
(15 patients) – 47.6 and 23.8% in the ORC and LRC Ureteroileal Surgery 2 (100)
groups respectively (p < 0.05). In 23 (54.8%) patients anastomosis
failure
90-day complications were observed – 14 (66.7%) and
9 (42.9%) after open and laparoscopic RC respectively
(p = 0.04). In each group 30-day mortality occurred in ileus) in three patients] and LRC (one patient both in
1 patient (p = 0.6). Distribution of patients according to the anastomotic ureteroileal urinary leakage and intestinal
grade of complications and time of their development is anastomotic leakage) groups respectively (p = 0.65). No
presented in Table 4, and according to the type of event cases of conversion to open surgery and no perioperative
and treatment strategy in Table 5. mortalities were reported.
Reoperation was performed in 4 (19.0%) and 2 (9.0%) We did not find significant difference between the
of the patients in the ORC [anastomotic ureteroileal groups in neither intraoperative (p = 0.7) nor 30-day
urinary leakage in one patient, pelvic abscess in one (p = 0.55) complications with grade 3 and more.
patient, and intestinal anastomotic failure (leakage or Three patients (14.3%) in the ORC group and 2 (9.5%)
in the LRC group required repeated hospitalization in
90 days after initial surgery (p = 0.65). The reason was
Table 3: Pathological data
grade 3 complications – acute upper urinary tract infec-
Median value tion (one patient in each group), ileal obstruction (one
Pathologic outcome LRC (n = 21) ORC (n = 21)
pT stage patient in each group), and pelvic abscess (one patient
pT1, n (%) 3 (14.3) 1 (4.8) in the ORC group).
pT2, n (%) 6 (28.5) 6 (28.5)
pT3-4, n (%) 12 (57.2) 14 (66.7) DISCUSSION
Removed lymph nodes, n (range) 14 (5–22) 15 (8–27) Historically, RC has been associated with the highest risk
pN+, n (%) 5 (23.8) 6 (28.5) of morbidity and mortality compared to all other major
Positive surgical margine, n (%) 2 (9.5) 2 (9.5)
LRC: Laparoscopic radical cystectomy; ORC: Open radical urologic procedures, particularly in the more elderly
cystectomy population. Standardized reports on complications after
ORC using the validated Clavien reporting system reveal
Table 4: Postoperative data disappointingly high complication and mortality rates –
from 26 to 64% and 1 to 7% respectively. 13-16
Median value
Value LRC (n = 21) ORC (n = 21) Until recently, there has been a dearth in standardized
30-day complications reporting of complications after RC. Only 2% of reports
Grade 0, n (%) 16 (76.1) 11 (52.3) (73 open series and 36 minimally invasive series) from
Grade 1 and 2, n (%) 2 (9.5) 6 (28.5) 1995 to 2005 met at least nine of the critical reporting
Grade 3–5, n (%) 3 (14.2) 4 (19.0) elements in surgical outcomes according to Donat. 17
90-day complications A lot of studies demonstrated the unmet need for
Grade 0, n (%) 12 (57.1) 7 (33.3) treatment of MIBC in terms of safety and efficacy. The
Grade 1 and 2, n (%) 3 (14.2) 7 (33.3) purpose of introduction of the minimally invasive
Grade 3–5, n (%) 6 (28.5) 7 (33.3)
90-day readmission rate, n (%) 2 (9.5) 3 (14.2) approach was to improve operative, pathological, and
LRC: Laparoscopic radical cystectomy; ORC: Open radical short-term clinical outcomes to the open approach.
cystectomy According to recent data, LRC suggests that operative
World Journal of Laparoscopic Surgery, May-August 2016;9(2):51-57 53