Page 84 - World Journal of Laparoscopic Surgery
P. 84
Laparoscopic Revision of Benign Hepaticojejunostomy Stricture
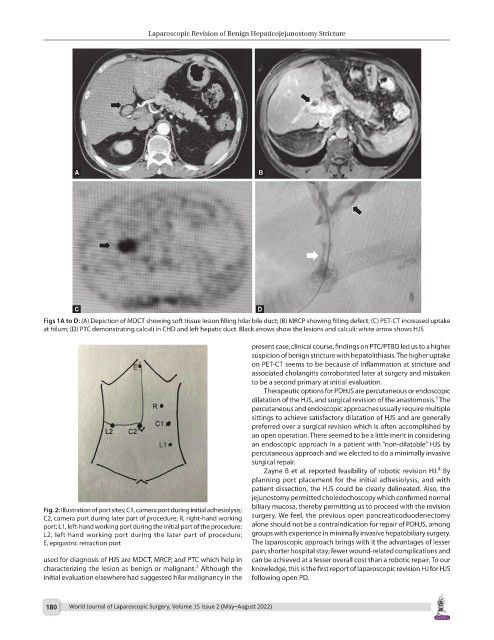
Figs 1A to D: (A) Depiction of MDCT showing soft tissue lesion filling hilar bile duct; (B) MRCP showing filling defect; (C) PET-CT increased uptake
at hilum; (D) PTC demonstrating calculi in CHD and left hepatic duct. Black arrows show the lesions and calculi; white arrow shows HJS
present case, clinical course, findings on PTC/PTBD led us to a higher
suspicion of benign stricture with hepatolithiasis. The higher uptake
on PET-CT seems to be because of inflammation at stricture and
associated cholangitis corroborated later at surgery and mistaken
to be a second primary at initial evaluation.
Therapeutic options for PDHJS are percutaneous or endoscopic
3
dilatation of the HJS, and surgical revision of the anastomosis. The
percutaneous and endoscopic approaches usually require multiple
sittings to achieve satisfactory dilatation of HJS and are generally
preferred over a surgical revision which is often accomplished by
an open operation. There seemed to be a little merit in considering
an endoscopic approach in a patient with “non-dilatable” HJS by
percutaneous approach and we elected to do a minimally invasive
surgical repair.
4
Zayne B et al. reported feasibility of robotic revision HJ. By
planning port placement for the initial adhesiolysis, and with
patient dissection, the HJS could be clearly delineated. Also, the
jejunostomy permitted choledochoscopy which confirmed normal
biliary mucosa, thereby permitting us to proceed with the revision
Fig. 2: Illustration of port sites; C1, camera port during initial adhesiolysis;
C2, camera port during later part of procedure; R, right-hand working surgery. We feel, the previous open pancreaticoduodenectomy
port; L1, left-hand working port during the initial part of the procedure; alone should not be a contraindication for repair of PDHJS, among
L2, left-hand working port during the later part of procedure; groups with experience in minimally invasive hepatobiliary surgery.
E, epigastric retraction port The laparoscopic approach brings with it the advantages of lesser
pain; shorter hospital stay; fewer wound-related complications and
used for diagnosis of HJS are MDCT, MRCP, and PTC which help in can be achieved at a lesser overall cost than a robotic repair. To our
2
characterizing the lesion as benign or malignant. Although the knowledge, this is the first report of laparoscopic revision HJ for HJS
initial evaluation elsewhere had suggested hilar malignancy in the following open PD.
180 World Journal of Laparoscopic Surgery, Volume 15 Issue 2 (May–August 2022)