The signs and symptoms of ovarian torsion can vary, and some individuals may not experience any symptoms at all. However, some common signs and symptoms of ovarian torsion include:
Sudden and severe lower abdominal pain on one side: This is the most common symptom of ovarian torsion. The pain can be intermittent or constant, and it may worsen with movement.
Nausea and vomiting: Individuals with ovarian torsion may experience nausea and vomiting, which can be severe in some cases.
Fever: A fever can be a sign of infection, which can occur as a complication of ovarian torsion.
Abnormal vaginal bleeding: Some individuals with ovarian torsion may experience abnormal vaginal bleeding, such as heavy bleeding or bleeding between periods.
Pain during intercourse: Ovarian torsion can cause pain during sexual intercourse.
Tenderness in the lower abdomen: The affected ovary may be tender to the touch.
Difficulty urinating: Ovarian torsion can cause pressure on the bladder, leading to difficulty urinating or increased frequency of urination.
It is essential to seek medical attention if you experience any of these symptoms, as ovarian torsion is a medical emergency that requires prompt diagnosis and treatment.
The diagnosis of ovarian torsion can be challenging, as the symptoms can be similar to other gynecological conditions. However, there are several diagnostic tests that healthcare providers can use to identify ovarian torsion. These tests include:
Pelvic examination: A pelvic exam can help identify any tenderness or swelling in the pelvic region, which can be a sign of ovarian torsion.
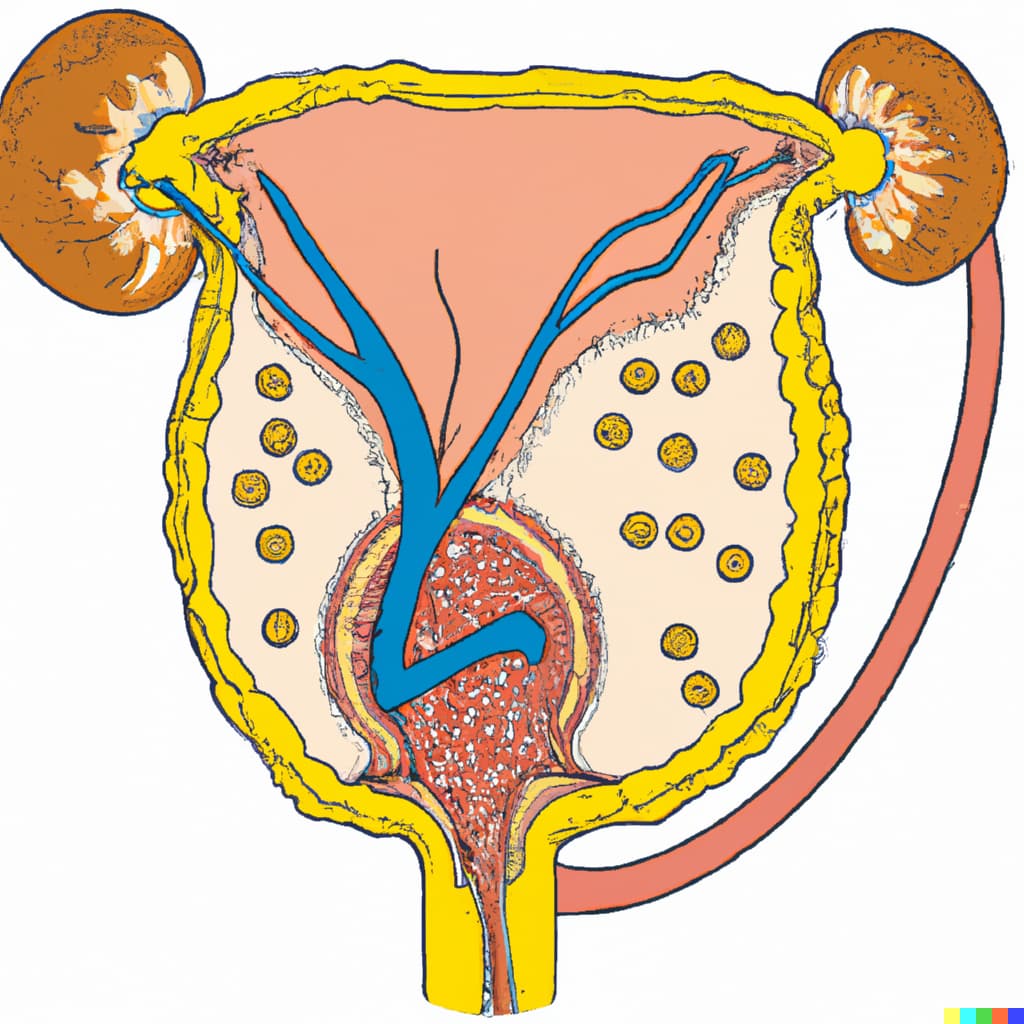
Imaging tests: Imaging tests, such as transvaginal ultrasound or computed tomography (CT) scan, can help visualize the ovaries and detect any abnormalities, such as twisting or enlargement.
Doppler ultrasound: This test can evaluate blood flow to the ovary and can help differentiate between ovarian torsion and other conditions, such as ovarian cysts.
Blood tests: Blood tests, such as a complete blood count (CBC) or C-reactive protein (CRP), can help identify signs of infection or inflammation.
If a healthcare provider suspects ovarian torsion, they may recommend further testing or refer the individual to a gynecologist or surgeon for additional evaluation. In some cases, laparoscopy, a minimally invasive surgical procedure, may be required to confirm the diagnosis and treat the condition.
Ovarian torsion is a gynecological emergency that can result in various complications, including:
Ovarian necrosis: Ovarian torsion can result in a lack of blood supply to the ovary, leading to tissue death or necrosis. This can cause long-term fertility reduction.
Hemorrhage: The twisting of the ovary can cause damage to the ovarian blood vessels, resulting in internal bleeding.
Infection: Ovarian torsion can lead to infection, especially if the necrotic tissue becomes infected or if surgery is required to treat the condition.
Peritonitis: If the necrotic ovary ruptures, it can lead to peritonitis or inflammation of the lining of the abdominal cavity.
Sepsis: If the infection becomes systemic, it can lead to sepsis, a life-threatening condition that requires immediate medical attention.
Bowel obstruction: In rare cases, ovarian torsion can lead to bowel obstruction due to adhesions or scar tissue formation in the pelvis.
It is essential to recognize the symptoms of ovarian torsion and seek immediate medical attention to prevent these complications. Early diagnosis and prompt treatment are crucial in preserving ovarian function and preventing long-term complications.
The laparoscopic management of ovarian torsion typically involves the following steps:
Anesthesia: The patient is placed under general anesthesia, and the surgical team prepares the patient for surgery.
Positioning: The patient is placed in a supine position with legs apart to allow for access to the pelvis.
Trocar placement: A laparoscope and other surgical instruments are inserted through small incisions in the abdomen, known as trocars.
Inspection of the pelvis: The laparoscope is used to inspect the pelvic area and visualize the twisted ovary.
Detorsion of the ovary: The surgeon detorses the ovary by carefully untwisting it to restore blood flow to the affected area.
Assessment of ovarian viability: The surgeon evaluates the ovary's viability by assessing its color, texture, and pulsatility. If the ovary appears necrotic or non-viable, the surgeon may need to remove it.
Ovarian cystectomy: If the torsion was caused by an ovarian cyst, the surgeon may perform a cystectomy to remove the cyst and prevent recurrence.
Hemostasis: The surgical team ensures hemostasis or the cessation of bleeding.
Closure of incisions: The surgical team closes the small incisions with sutures or surgical glue.
After the surgery, the patient is monitored in the recovery room and is typically discharged from the hospital within a few days. The patient may need to avoid strenuous activities for several weeks and follow up with their healthcare provider for postoperative care.
After laparoscopic surgery for ovarian torsion, it is essential to follow the postoperative care instructions provided by the healthcare provider. These instructions typically include:
Pain management: The patient may experience some pain and discomfort after surgery, and pain medication may be prescribed to manage the pain.
Activity restrictions: The patient may need to avoid strenuous activities, heavy lifting, and exercise for a few weeks after surgery. The healthcare provider may recommend walking or light activities to promote healing.
Diet: The healthcare provider may recommend a soft diet or liquids for the first few days after surgery to allow the digestive system to rest.
Incision care: The patient should keep the incision area clean and dry and avoid soaking in water or exposing it to direct sunlight. The healthcare provider may recommend applying an antibiotic ointment to the incision site.
Follow-up appointments: The patient should attend all scheduled follow-up appointments to monitor their recovery and ensure that there are no complications.
Emotional support: It is common to experience emotional distress after surgery, and patients may benefit from emotional support from family members, friends, or a mental health professional.
It is important to contact the healthcare provider immediately if the patient experiences any of the following symptoms:
Severe pain or bleeding
Signs of infection, such as fever, chills, or redness around the incision site
Nausea or vomiting that does not resolve
Difficulty urinating or blood in the urine
With proper postoperative care and follow-up, most patients can recover fully from laparoscopic surgery for ovarian torsion and resume their daily activities.