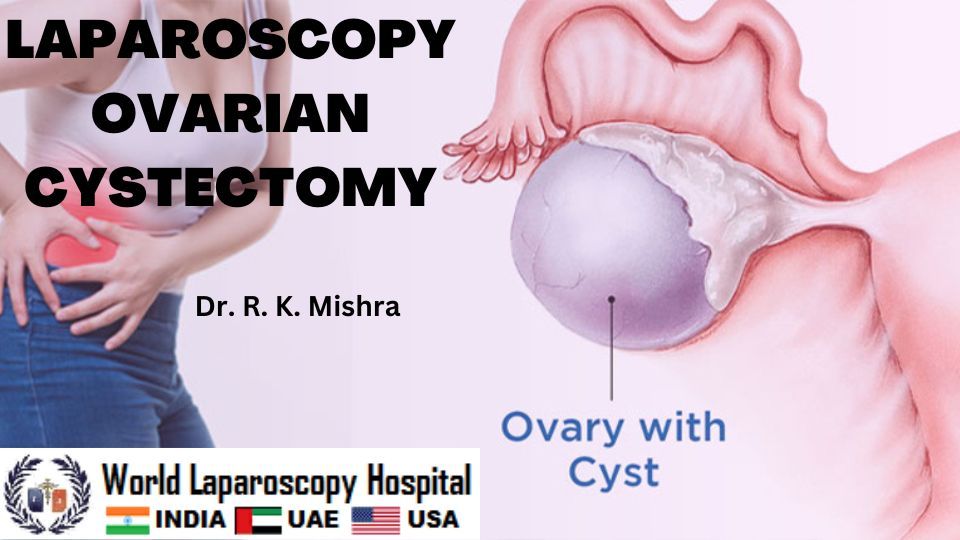
Laparoscopic ovarian cystectomy is a minimally invasive surgical procedure that involves the removal of an ovarian cyst through small incisions in the abdomen. This procedure is used to treat a variety of conditions, including endometriomas, dermoid cysts, and functional cysts. In this article, we will discuss the step-by-step process of performing a laparoscopic ovarian cystectomy.
Preoperative Preparation:
Before the surgery, the patient is required to undergo a thorough preoperative evaluation, including blood tests, imaging studies, and a physical examination. The patient should also be advised to avoid eating or drinking anything for at least 6-8 hours before the procedure.
Step-by-Step Procedure:
The patient is placed under general anesthesia. The anesthesiologist monitors the patient's vital signs throughout the procedure.
Placement of Trocars:
The surgeon creates small incisions in the abdomen, through which trocars are inserted. Trocars are long, thin instruments that provide access to the abdominal cavity. Typically, a laparoscope (a long, thin tube with a camera and light source) is inserted through one of the trocars. The other trocars are used to insert other surgical instruments.
Inspection of the Abdominal Cavity:
The surgeon inspects the abdominal cavity using the laparoscope. The abdominal organs, including the ovaries, are visualized. The surgeon identifies the cyst and evaluates its size, location, and characteristics.
Separation of the Cyst:
Using a scalpel or electrocautery, the surgeon carefully separates the cyst from the surrounding ovarian tissue. The surgeon takes care to preserve as much healthy ovarian tissue as possible. The cyst is then removed from the abdomen.
Hemostasis:
Once the cyst has been removed, the surgeon uses electrocautery or other techniques to achieve hemostasis, or control of bleeding, in the ovarian tissue. This is important to prevent bleeding and other complications.
Closure of Incisions:
After the procedure, the surgeon removes the trocars and closes the incisions using sutures or surgical glue. The patient is then transferred to the recovery room.
Postoperative Care:
The patient is monitored in the recovery room for several hours to ensure that there are no complications. The patient is typically able to go home on the same day as the surgery. The surgeon will provide postoperative instructions, including advice on wound care, pain management, and activity restrictions. The patient will typically need to avoid strenuous activity for several weeks after the surgery.
Possible continuation:
Complications:
As with any surgical procedure, laparoscopic ovarian cystectomy carries some risks and potential complications. Some of these include:
- Bleeding: In rare cases, there may be excessive bleeding during or after the surgery that may require additional intervention.
- Infection: There is a small risk of infection at the incision sites or in the abdominal cavity, which can cause fever, pain, and other symptoms.
- Damage to surrounding organs: During the surgery, there is a risk of unintentionally damaging nearby organs, such as the bladder, ureter, or bowel.
- Recurrence: Although the cyst is removed during the surgery, there is a small chance that it may recur in the future.
Tips for Success:
Here are some tips to increase the success of a laparoscopic ovarian cystectomy:
- Choose an experienced and skilled surgeon who is trained in laparoscopic surgery.
- Use appropriate surgical technique and instruments to minimize the risk of complications.
- Ensure proper patient preparation and follow-up care to minimize the risk of infection and other postoperative complications.
- Use appropriate hemostatic measures to control bleeding during the surgery.
- Consider the size and location of the cyst when selecting the surgical approach and instruments.
After a laparoscopic ovarian cystectomy, the patient will typically be advised to return for follow-up appointments with their surgeon. This is important to monitor the healing process and ensure that there are no complications.
During the follow-up appointments, the surgeon may perform imaging studies, such as ultrasound or MRI, to evaluate the status of the ovaries and ensure that there is no recurrence of the cyst. The surgeon may also perform a physical exam and ask the patient about any symptoms they may be experiencing.
The patient may be advised to avoid certain activities, such as heavy lifting or strenuous exercise, for several weeks after the surgery. The surgeon will provide specific instructions based on the patient's individual situation.
The patient should also be aware of signs of potential complications, such as fever, pain, or abnormal discharge from the incision sites. If any of these symptoms occur, the patient should contact their surgeon right away.
Long-Term Outlook:
In most cases, laparoscopic ovarian cystectomy is a successful and effective treatment for ovarian cysts. The patient can expect to experience a faster recovery time and less pain compared to traditional open surgery. However, it is important to note that there is a risk of recurrence of the cyst in the future. The patient should continue to undergo regular monitoring by their healthcare provider to ensure that there are no new cysts or other complications. Additionally, in some cases, the removal of an ovarian cyst may affect fertility. The patient should discuss any concerns about fertility with their healthcare provider before the surgery.
Recovery:
After a laparoscopic ovarian cystectomy, the patient will typically experience some pain and discomfort, which can be managed with pain medications prescribed by their healthcare provider. The patient may also experience some bloating and nausea, which are common after abdominal surgery. The patient may be able to go home on the same day as the surgery, or they may need to stay in the hospital for a short period of time for observation.
The patient will need to rest and avoid strenuous activities for several weeks after the surgery. They may also need to take time off work, depending on the nature of their job. The healthcare provider will provide specific instructions on wound care, including how to keep the incision sites clean and dry, and when to change dressings. The patient should also avoid sexual activity for several weeks after the surgery, to allow the incisions to heal properly. The healthcare provider will schedule follow-up appointments to monitor the patient's recovery and ensure that there are no complications.
Diet:
After the surgery, the patient may have some nausea or vomiting, which can make it difficult to eat. The healthcare provider may recommend a light diet, such as clear liquids or broth, for the first day or two after the surgery. The patient can then gradually return to a normal diet as tolerated. The patient should avoid fatty or spicy foods, which can irritate the digestive system and cause discomfort. They should also drink plenty of fluids to prevent dehydration.
Complications:
As with any surgical procedure, laparoscopic ovarian cystectomy carries a risk of complications. The following are some of the potential complications and how they can be managed:
- Infection: Infection can occur at the incision sites or in the abdominal cavity. The symptoms may include fever, chills, redness, swelling, and drainage from the incisions. In most cases, antibiotics are prescribed to treat the infection. In some cases, drainage of the infected fluid may be necessary.
- Bleeding: Bleeding can occur during or after the surgery, and can sometimes require additional intervention. During the surgery, the surgeon will use hemostatic measures to control bleeding, such as sutures or electrocautery. If bleeding occurs after the surgery, the patient may need to be taken back to the operating room for further treatment.
- Damage to surrounding organs: During the surgery, there is a risk of unintentional damage to nearby organs, such as the bladder, bowel, or ureter. This can cause pain, bleeding, or other complications. If damage to these organs is suspected, further evaluation and treatment may be necessary.
- Recurrence of the cyst: Although the cyst is removed during the surgery, there is a risk of recurrence in the future. The patient should continue to undergo regular monitoring by their healthcare provider to ensure that there are no new cysts or other complications.
- Adhesions: Adhesions are bands of scar tissue that can form after surgery. Adhesions can cause pain and other complications. In some cases, further surgery may be necessary to remove the adhesions.
- Anesthesia-related complications: General anesthesia can carry a small risk of complications, such as allergic reactions, breathing difficulties, or heart problems. The anesthesiologist will monitor the patient closely during the surgery to minimize the risk of complications.
- Thrombosis: Surgery can increase the risk of blood clots forming in the veins of the legs or pelvis. This can cause pain, swelling, or redness in the affected leg. To minimize the risk of thrombosis, the healthcare provider may recommend the use of compression stockings or blood-thinning medications.
- Urinary problems: Surgery near the bladder or ureters can cause temporary problems with urination, such as difficulty passing urine or urinary tract infections. These problems usually resolve on their own within a few days or weeks.
- Shoulder pain: During laparoscopic surgery, carbon dioxide gas is used to inflate the abdomen, which can cause referred pain in the shoulders. This usually resolves within a few hours after the surgery.
- Endometriomas: These cysts are caused by endometriosis, a condition in which tissue that normally lines the uterus grows outside of it. Endometriomas can be more difficult to remove completely, and there is a higher risk of recurrence after surgery.
- Dermoid cysts: These cysts can contain a variety of tissues, including hair, skin, and teeth. Removing these cysts can be more challenging, and there is a risk of rupturing the cyst during surgery, which can cause inflammation and infection.
- Functional cysts: These cysts are caused by changes in the normal menstrual cycle and typically resolve on their own without treatment. In some cases, however, they may grow large enough to cause discomfort or other symptoms, requiring surgery. These cysts are generally easier to remove and have a lower risk of complications.
Overall, the risk of complications and the difficulty of the surgery will depend on the size, location, and type of cyst, as well as the patient's individual health status and medical history.
To manage these complications, the healthcare provider will take appropriate measures to minimize the risks and provide prompt treatment if necessary. It is important for the patient to communicate any symptoms or concerns with their healthcare provider.
In some cases, further surgery or other interventions may be necessary to manage complications. The healthcare provider will provide the patient with specific instructions on wound care, pain management, and activity restrictions to minimize the risk of complications and promote a smooth recovery.
Conclusion:
Laparoscopic ovarian cystectomy is a minimally invasive surgical procedure that can provide effective treatment for ovarian cysts. The patient can expect to experience some pain and discomfort after the surgery, but this can be managed with pain medications.
The patient will need to rest and avoid strenuous activities for several weeks after the surgery. They will also need to follow specific instructions on wound care and diet.
Although the procedure is generally safe, there is a risk of complications, which the healthcare provider will take appropriate measures to minimize. With proper care and monitoring, the patient can expect to have an excellent long-term outcome after laparoscopic ovarian cystectomy.