Introduction:
The field of medicine has seen remarkable advancements over the years, and one of the most significant revolutions in gynecology has been the advent of laparoscopic hysterectomy. This minimally invasive surgical procedure has not only transformed the way hysterectomies are performed but has also improved patient outcomes, reduced recovery times, and enhanced the quality of life for countless women around the world. In this comprehensive article, we will delve into the history, techniques, benefits, and future prospects of laparoscopic hysterectomy.
The Historical Context
The roots of laparoscopic surgery can be traced back to the early 20th century when the first laparoscope was developed. However, it was not until the late 20th century that laparoscopic techniques were applied to gynecological procedures, including hysterectomy. Traditional open surgery, with its larger incisions, longer hospital stays, and extended recovery times, was the norm for decades. But as laparoscopic technology and surgical skills advanced, a shift towards minimally invasive procedures began to take place.
The Laparoscopic Hysterectomy Procedure
Laparoscopic hysterectomy, also known as minimally invasive hysterectomy, involves the removal of the uterus through small incisions made in the abdominal wall. There are different approaches to this surgery, each with its unique advantages, including:
1. Laparoscopic-Assisted Vaginal Hysterectomy (LAVH): In LAVH, the laparoscope is used to assist in the removal of the uterus through the vaginal canal, reducing the need for a large abdominal incision.
2. Total Laparoscopic Hysterectomy (TLH): TLH is performed entirely through small abdominal incisions using a laparoscope, without the need for a vaginal incision.
3. Robot-Assisted Laparoscopic Hysterectomy: This approach incorporates robotic assistance to enhance the surgeon's precision and control during the procedure.
4. Single-Incision Laparoscopic Hysterectomy: In SILH, the entire surgery is performed through a single incision, usually in the belly button, resulting in minimal scarring.
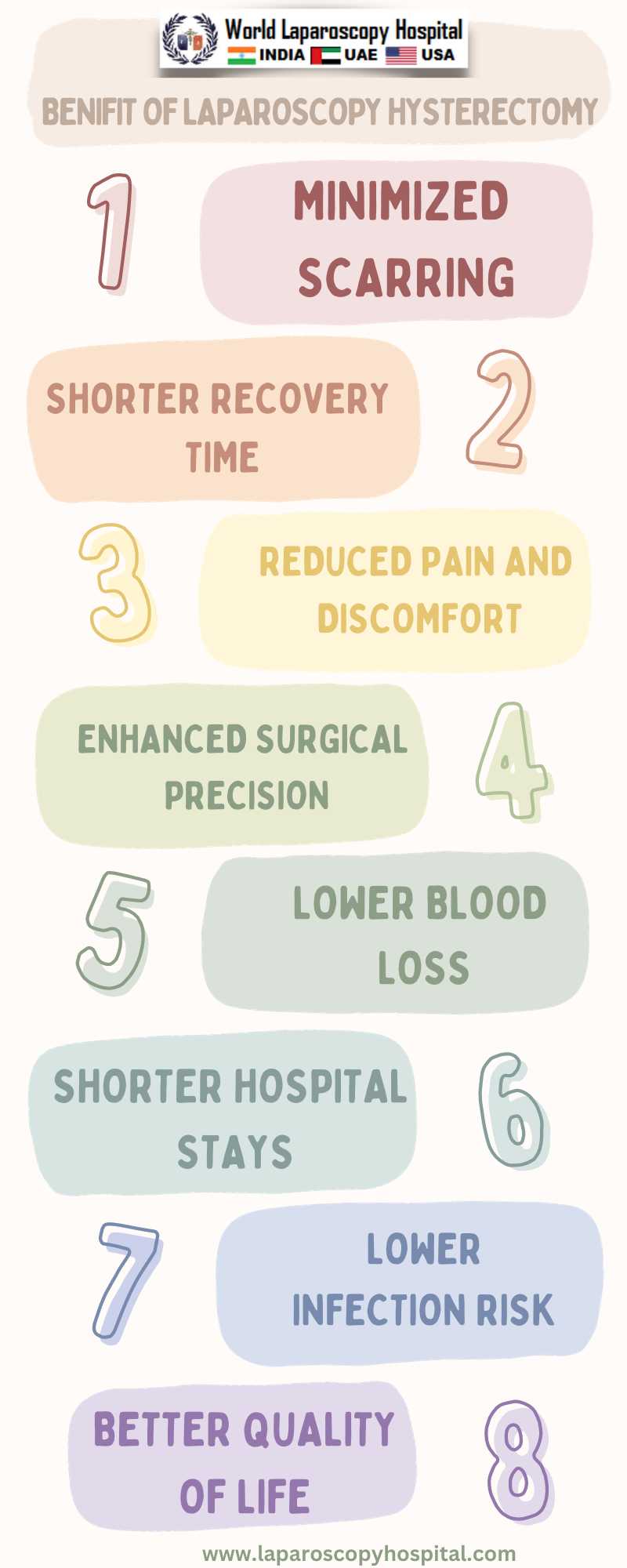
The Benefits of Laparoscopic Hysterectomy
1. Minimized Scarring: The most apparent benefit of laparoscopic hysterectomy is the reduction in scarring. Small incisions result in less visible scarring and reduced risk of infection.
2. Shorter Hospital Stays: Patients undergoing laparoscopic hysterectomy typically have shorter hospital stays, often going home on the same day or the day after surgery, as compared to traditional open surgery.
3. Quicker Recovery: The recovery time for patients is significantly shorter, allowing them to return to their daily activities and work sooner.
4. Less Pain: Minimally invasive techniques generally result in less postoperative pain and discomfort.
5. Reduced Blood Loss: Laparoscopic procedures are associated with less intraoperative blood loss, reducing the need for blood transfusions.
6. Lower Infection Risk: Smaller incisions and reduced exposure to the external environment result in a lower risk of infection.
7. Improved Cosmetic Outcomes: The smaller scars are more cosmetically appealing and contribute to improved body image and self-esteem.
8. Better Quality of Life: Laparoscopic hysterectomy often leads to better postoperative quality of life, as patients experience less pain and a quicker return to their usual activities.
9. Enhanced Visualization: The laparoscope provides surgeons with a magnified, high-definition view of the surgical site, enabling precision and accuracy.
10. Reduced Risk of Adhesions: Laparoscopic techniques are associated with a lower risk of postoperative adhesions, which can cause complications in the long term.
Future Prospects
The future of laparoscopic hysterectomy looks promising, with ongoing research and advancements in technology. This includes the integration of augmented reality and artificial intelligence into surgical procedures, which may further enhance the precision and safety of the surgery. Additionally, continued training and education for gynecological surgeons in laparoscopic techniques will help expand the availability of this minimally invasive approach to women in need of hysterectomies.
Conclusion:
Laparoscopic hysterectomy has truly been a surgical revolution in gynecology. This minimally invasive approach has not only reduced the physical and emotional burdens on patients but has also raised the bar for surgical precision and outcomes. As technology and expertise continue to advance, we can expect further refinements in laparoscopic techniques, ultimately benefiting women worldwide. The journey from open surgery to minimally invasive laparoscopic procedures is a testament to the evolution of medical science and its unwavering commitment to enhancing the lives of patients.