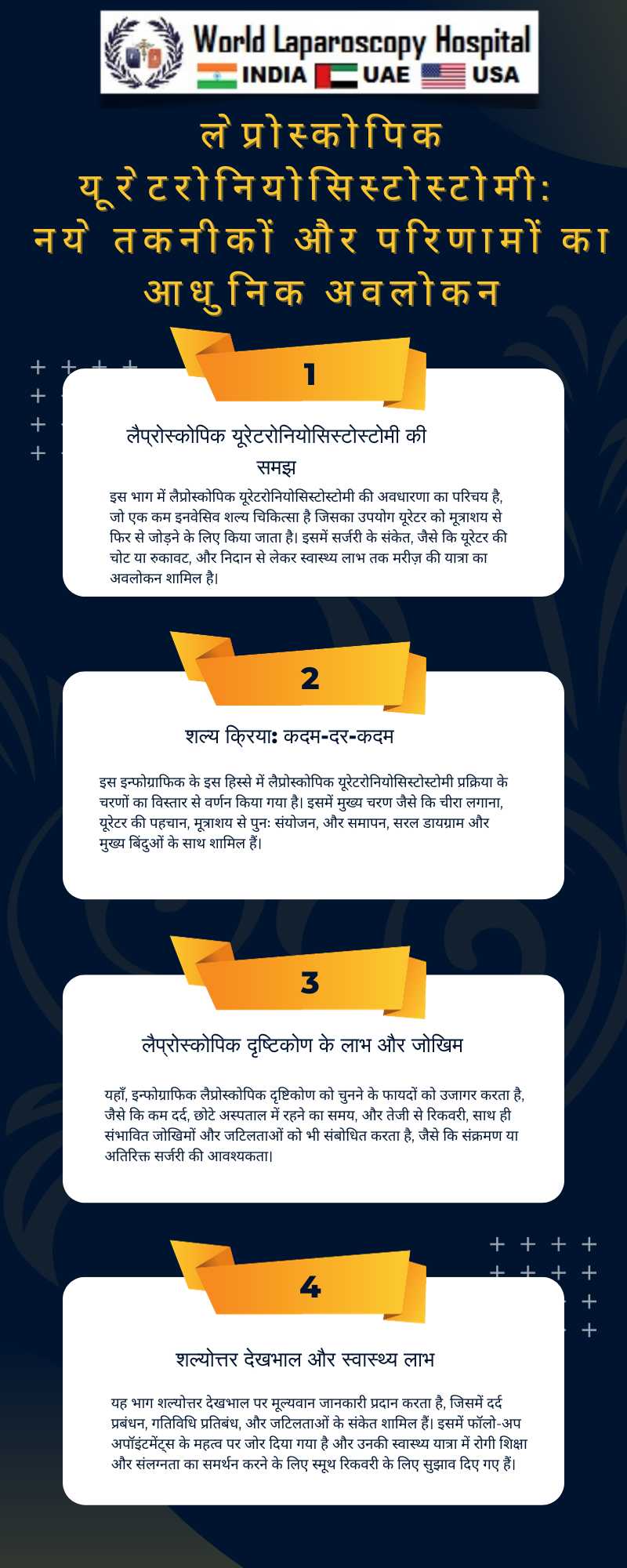
The landscape of surgical procedures has been significantly revolutionized with the introduction and advancement of minimally invasive techniques. Among these, laparoscopic ureteroneocystostomy stands out as a remarkable example of how surgical interventions have evolved, particularly in urology. This procedure, which involves the reattachment of the ureter to the bladder, is a testament to the precision and efficiency that modern surgery can achieve.
Historical Perspective and Evolution
Traditionally, ureteroneocystostomy was performed through open surgery, which often resulted in longer hospital stays, increased pain, and more significant scarring for the patient. However, the advent of laparoscopic techniques has transformed this landscape. The first laparoscopic ureteroneocystostomy was reported in the early 1990s, marking a significant milestone in minimally invasive urologic surgery.
Technological Integration
The integration of advanced technologies has been pivotal in the evolution of laparoscopic ureteroneocystostomy. High-definition cameras and refined laparoscopic instruments offer unparalleled precision and control. The use of robotics, such as the da Vinci Surgical System, further enhances the surgeon's dexterity, allowing for more precise suturing and manipulation of delicate tissues.
Patient-Centric Benefits
One of the most significant advantages of laparoscopic ureteroneocystostomy is the reduced impact on the patient. The minimally invasive nature of the procedure results in smaller incisions, leading to less postoperative pain and quicker recovery times. This approach also minimizes the risk of infections and postoperative complications, contributing to better overall outcomes for patients.
Skill and Training
The successful implementation of laparoscopic ureteroneocystostomy hinges on the skill and expertise of the surgeon. It requires a comprehensive understanding of the anatomy, as well as proficiency in laparoscopic techniques. Consequently, there has been an emphasis on specialized training and simulation-based learning to equip surgeons with the necessary skills.
Current Challenges and Future Directions
Despite its advantages, laparoscopic ureteroneocystostomy poses certain challenges. The procedure requires a high level of technical skill and experience, which can be a limiting factor in its widespread adoption. Moreover, the cost of equipment and maintenance of laparoscopic and robotic systems can be prohibitive for some healthcare facilities.
Looking towards the future, ongoing research and innovation are likely to address these challenges. The development of more cost-effective laparoscopic instruments and enhanced training programs are expected to make this technique more accessible. Furthermore, advancements in surgical techniques and technology, such as augmented reality and artificial intelligence, are poised to further refine and improve the outcomes of laparoscopic ureteroneocystostomy.
Conclusion:
Laparoscopic ureteroneocystostomy exemplifies the remarkable advancements in minimally invasive surgery. It offers significant benefits to patients, including reduced recovery times and decreased morbidity. As technology continues to evolve and surgical techniques are refined, this procedure is likely to become more commonplace, further transforming the landscape of urological surgery.