In the dynamic world of surgical oncology, the laparoscopic inguinal lymph node dissection represents a significant stride in the realm of precision and progress. This minimally invasive procedure, an evolution of the traditional open lymph node dissection, is a testament to the relentless pursuit of surgical excellence and patient-centered care. It's an art form that harmonizes the delicate balance between comprehensive cancer treatment and the minimization of surgical trauma.
Understanding the Procedure
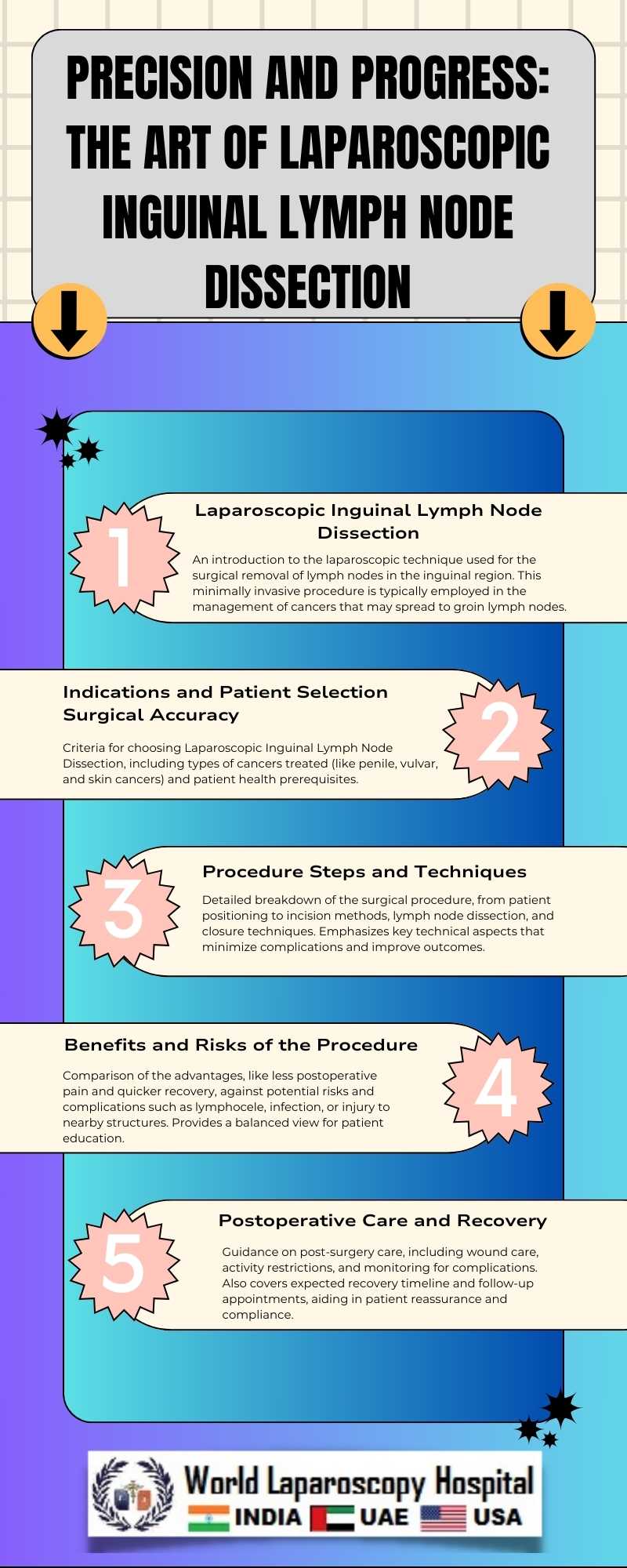
Laparoscopic inguinal lymph node dissection involves the removal of lymph nodes in the groin region through small incisions, using laparoscopic instruments and techniques. This approach is primarily employed in the management of malignancies such as melanoma, penile, vulvar, and some types of urological and gynecological cancers, where the inguinal lymph nodes are a common site for metastasis.
Technological Marvels and Surgical Precision
The procedure epitomizes surgical precision, facilitated by advanced laparoscopic equipment that allows surgeons to navigate complex anatomical regions with enhanced visibility and dexterity. High-definition cameras provide magnified views of the surgical field, ensuring meticulous dissection and preservation of vital structures such as nerves and blood vessels. The use of ultrasonic shears and energy devices has further refined the technique, allowing for more efficient and hemostatic tissue manipulation.
Patient-Centered Benefits
The benefits of this laparoscopic technique extend far beyond its oncological efficacy. Patients experience significantly reduced postoperative pain, smaller incisions leading to minimal scarring, and a lower risk of complications like wound infections and lymphedema. These advantages translate into shorter hospital stays, quicker recovery times, and an overall improved quality of life.
Training and Skill: The Hallmarks of Mastery
Mastering laparoscopic inguinal lymph node dissection demands a high level of skill and training. Surgeons must navigate a steep learning curve to become adept in this technique. This involves an intricate understanding of the inguinal anatomy, proficiency in laparoscopic skills, and the ability to manage intraoperative challenges. Training programs and workshops, combined with simulation and hands-on experience, play a crucial role in disseminating this expertise.
Challenges and Future Directions
Despite its benefits, the procedure is not devoid of challenges. The complex anatomy of the inguinal region, coupled with the proximity to vital structures, requires meticulous surgical planning and execution. Moreover, the adoption of this technique is limited by its availability only in specialized centers and by surgeons with advanced laparoscopic skills.
The future of laparoscopic inguinal lymph node dissection is bright, with ongoing research focusing on further refinements. Innovations like robotic-assisted surgery, fluorescence imaging, and real-time lymphatic mapping are on the horizon. These advancements promise to enhance the precision and safety of the procedure, potentially making it accessible to a broader range of patients and settings.
Conclusion
Laparoscopic inguinal lymph node dissection stands at the intersection of precision and progress in surgical oncology. It encapsulates the relentless pursuit of surgical excellence, balancing oncological radicality with patient welfare. As technology advances and surgical skills evolve, this technique will continue to play a pivotal role in the management of cancers with inguinal lymph node involvement, symbolizing a future where surgical interventions are not only effective but also empathetic.