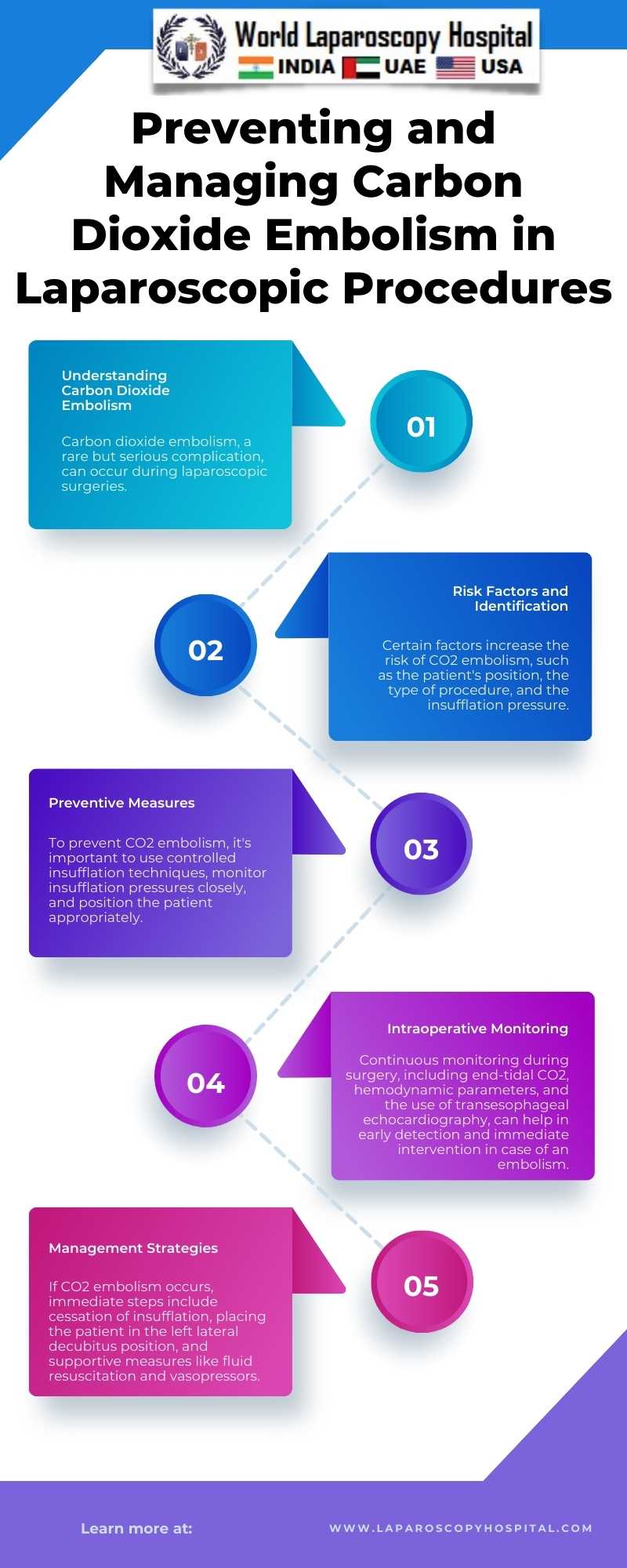
Laparoscopic surgery, a minimally invasive procedure, has gained immense popularity due to its advantages like reduced pain, shorter hospital stays, and quicker recovery. However, it introduces unique complications, one of which is carbon dioxide (CO2) embolism. This rare but potentially fatal complication occurs when CO2 gas used for insufflation enters the vascular system. Understanding, preventing, and managing CO2 embolism is crucial for the safety of patients undergoing laparoscopic procedures.
Pathophysiology of CO2 Embolism:
During laparoscopy, CO2 gas is used to create pneumoperitoneum, enhancing visibility and operative space. CO2 embolism occurs when the gas inadvertently enters the vascular system, usually through a vein. It can lead to a gas lock in the right ventricle, impairing cardiac output, and decreasing venous return. The gas can also travel to the pulmonary vasculature, causing a reduction in pulmonary blood flow and gas exchange, leading to hypoxemia and hypercapnia.
Prevention Strategies:
1. Proper Patient Positioning: Patient positioning is critical. The Trendelenburg position should be cautiously used as it may increase the risk of venous air embolism.
2. Controlled Insufflation: Slow, controlled insufflation with initial low pressure can minimize the risk. Using an insufflator with a pressure limit and flow rate control is advisable.
3. Veress Needle and Trocar Placement: Correct placement of the Veress needle and trocars is essential. Aspiration and saline drop test should be performed to ensure correct placement.
4. Monitoring: Continuous intraoperative monitoring, including end-tidal CO2, hemodynamic parameters, and oxygen saturation, can help in early detection of an embolism.
5. Training and Experience: Surgeons should be well-trained in laparoscopic techniques. Experience plays a significant role in minimizing complications.
Management of CO2 Embolism:
1. Immediate Response: If CO2 embolism is suspected, the first step is to discontinue insufflation and deflate the pneumoperitoneum.
2. Cardiopulmonary Support: Basic life support measures should be initiated. This includes administering 100% oxygen to improve tissue oxygenation and managing hemodynamics with fluids and vasopressors if necessary.
3. Positional Maneuvers: Placing the patient in the left lateral decubitus and Trendelenburg position can help trap air in the apex of the right ventricle, preventing its entry into the pulmonary artery.
4. Advanced Cardiac Life Support (ACLS): If the patient develops cardiac arrest, ACLS protocols should be followed.
5. Definitive Care: In severe cases, hyperbaric oxygen therapy and cardiopulmonary bypass may be considered.
Conclusion:
While CO2 embolism in laparoscopic surgery is rare, its potential severity warrants a high degree of vigilance. Preventive strategies focusing on technique, patient positioning, and proper equipment use are crucial. Early recognition and prompt management are key to mitigating the adverse effects of this complication. Ongoing education and training in laparoscopic techniques remain pivotal for surgical teams to ensure patient safety and successful outcomes.