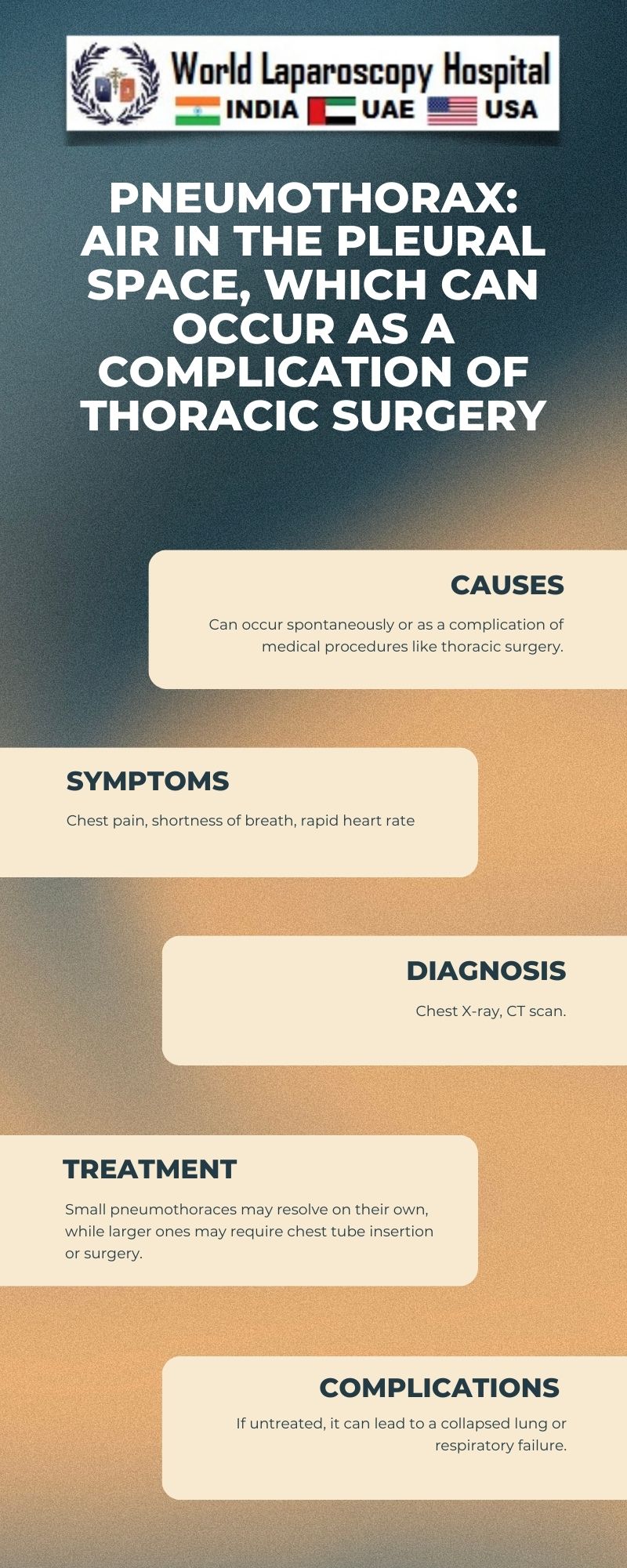
Pneumothorax: Air in the pleural space, which can occur as a complication of thoracic surgery
Introduction:
Pneumothorax, defined as the presence of air in the pleural space, can be a significant complication following thoracic surgery. This condition can range from asymptomatic to life-threatening, depending on the extent of lung collapse and the presence of underlying lung disease. In the context of thoracic surgery, pneumothorax can occur due to various factors, including surgical trauma to the lung tissue, barotrauma from positive pressure ventilation, and underlying lung pathology. Understanding the risk factors, clinical presentation, diagnosis, and management of postoperative pneumothorax is crucial for healthcare providers involved in thoracic surgery.
Risk Factors:
Several factors can increase the risk of developing pneumothorax following thoracic surgery. These include:
- Type of surgery: Certain procedures, such as lung resection (lobectomy, pneumonectomy), are associated with a higher risk of pneumothorax due to the manipulation and removal of lung tissue.
- Use of positive pressure ventilation: Mechanical ventilation can lead to barotrauma, causing alveolar rupture and air leakage into the pleural space.
- Underlying lung disease: Patients with pre-existing lung conditions, such as emphysema or cystic fibrosis, are at a higher risk of developing pneumothorax postoperatively.
- Smoking: Smoking is a significant risk factor for the development of lung disease, which can predispose individuals to pneumothorax.
- Previous pneumothorax: Patients with a history of pneumothorax are at an increased risk of recurrence following thoracic surgery.
Clinical Presentation:
The clinical presentation of postoperative pneumothorax can vary depending on the size of the pneumothorax and the underlying lung function. Common symptoms include:
- Sudden onset of chest pain, which may be sharp or stabbing in nature.
- Shortness of breath, especially with exertion.
- Decreased breath sounds on the affected side.
- Hypoxemia (low oxygen levels) and tachypnea (rapid breathing).
- Tachycardia (rapid heart rate) and cyanosis (bluish discoloration of the skin).
In some cases, especially with small pneumothoraces, patients may be asymptomatic, and the condition may only be detected on imaging studies performed for other reasons.
Diagnosis:
Diagnosing pneumothorax postoperatively requires a high index of suspicion, especially in patients with risk factors or suggestive symptoms. The following diagnostic modalities are commonly used:
- Chest X-ray: This is the initial imaging modality of choice for evaluating suspected pneumothorax. It can reveal the presence of air in the pleural space and the extent of lung collapse.
- CT scan: In cases where the diagnosis is uncertain or further characterization is needed, a CT scan of the chest can provide detailed images of the lung and pleural space.
- Ultrasound: Bedside ultrasound can be used to rapidly detect pneumothorax, especially in critically ill patients.
Management:
The management of postoperative pneumothorax depends on the size of the pneumothorax, the patient's symptoms, and the underlying lung function. Options include:
- Observation: Small, asymptomatic pneumothoraces may be managed conservatively with close observation and serial chest X-rays to ensure resolution.
- Needle aspiration or chest tube insertion: Larger or symptomatic pneumothoraces may require needle aspiration or chest tube insertion to evacuate the air and re-expand the lung.
- Surgery: In some cases, especially with persistent air leak or recurrent pneumothorax, surgical intervention may be necessary to repair the lung tissue and prevent future recurrences.
Prevention:
Preventing postoperative pneumothorax involves identifying and addressing modifiable risk factors. Strategies include:
- Minimizing surgical trauma: Surgeons should aim to minimize lung tissue manipulation and use gentle handling techniques during surgery.
- Lung protective ventilation: Using low tidal volumes and avoiding high airway pressures can reduce the risk of barotrauma.
- Smoking cessation: Encouraging patients to quit smoking before surgery can improve lung function and reduce the risk of complications.
- Postoperative care: Providing appropriate pain management and respiratory support in the postoperative period can help prevent complications such as atelectasis and pneumothorax.
Conclusion:
Pneumothorax is a known complication following thoracic surgery, with potentially serious consequences. Healthcare providers involved in thoracic surgery should be aware of the risk factors, clinical presentation, diagnosis, and management of postoperative pneumothorax to ensure timely recognition and appropriate intervention. By implementing preventive strategies and adopting a proactive approach to patient care, the incidence and severity of postoperative pneumothorax can be minimized, improving patient outcomes and quality of life.