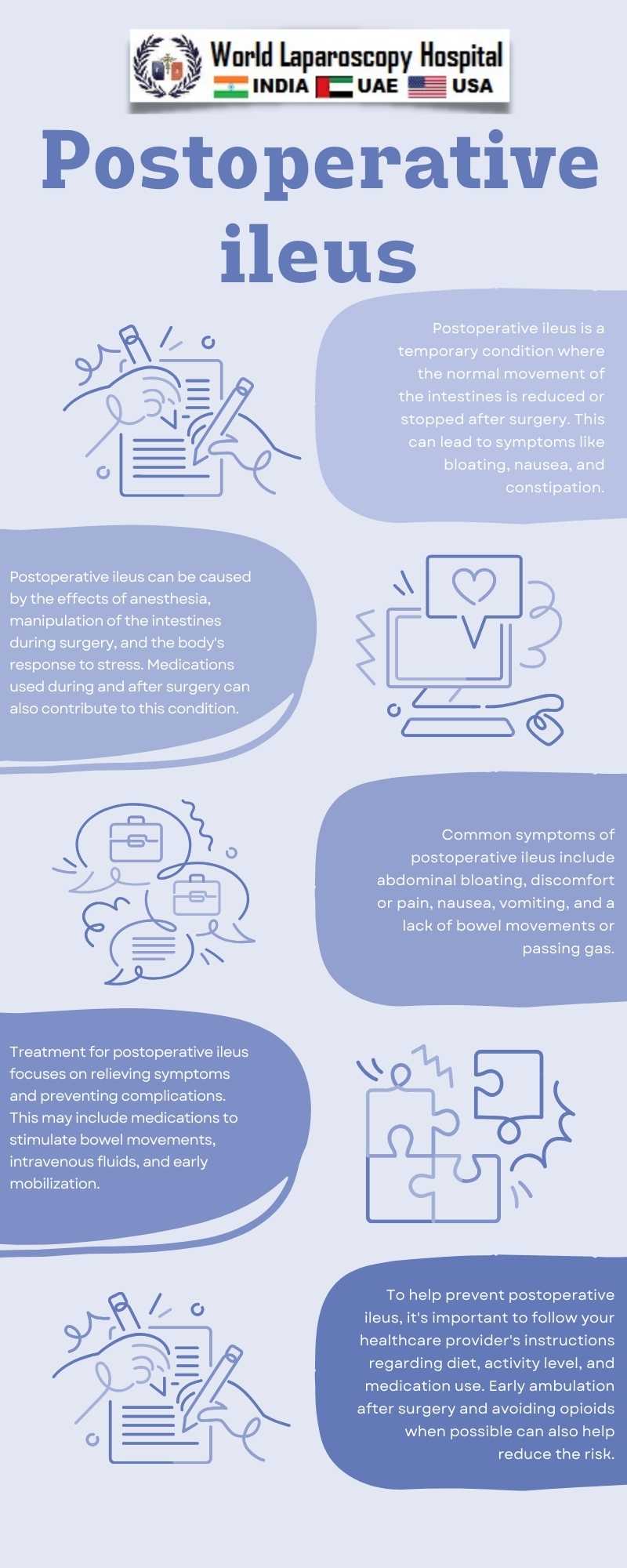
The exact mechanisms underlying postoperative ileus are not fully understood but are thought to involve a combination of local and systemic factors. Surgical trauma leads to inflammation and disruption of the normal neural and hormonal pathways that regulate bowel motility. Anesthesia and opioid pain medications further contribute to the development of ileus by affecting the function of the enteric nervous system and smooth muscle activity in the gastrointestinal tract.
The clinical presentation of postoperative ileus typically includes abdominal distention, lack of bowel sounds, nausea, vomiting, and delayed passage of flatus and stool. These symptoms can cause discomfort and distress to patients and may also result in complications such as dehydration, electrolyte imbalances, and aspiration pneumonia.
Management of postoperative ileus focuses on supportive care, early mobilization, and avoidance of factors that can exacerbate the condition. Patients are encouraged to ambulate as soon as possible after surgery to stimulate bowel motility and reduce the risk of ileus. Additionally, the use of opioid-sparing pain management strategies and the early initiation of enteral nutrition can help prevent and alleviate ileus.
In cases where conservative measures are ineffective, pharmacological interventions such as prokinetic agents may be considered to enhance bowel motility. Surgical interventions are rarely necessary and are reserved for patients with severe or refractory ileus.
Conclusion
Postoperative ileus is a temporary impairment of bowel motility that commonly occurs after abdominal surgery. While usually self-limiting, it can lead to significant morbidity if not managed effectively. Understanding the underlying mechanisms and implementing appropriate management strategies are essential in optimizing the outcomes of patients undergoing abdominal surgery.