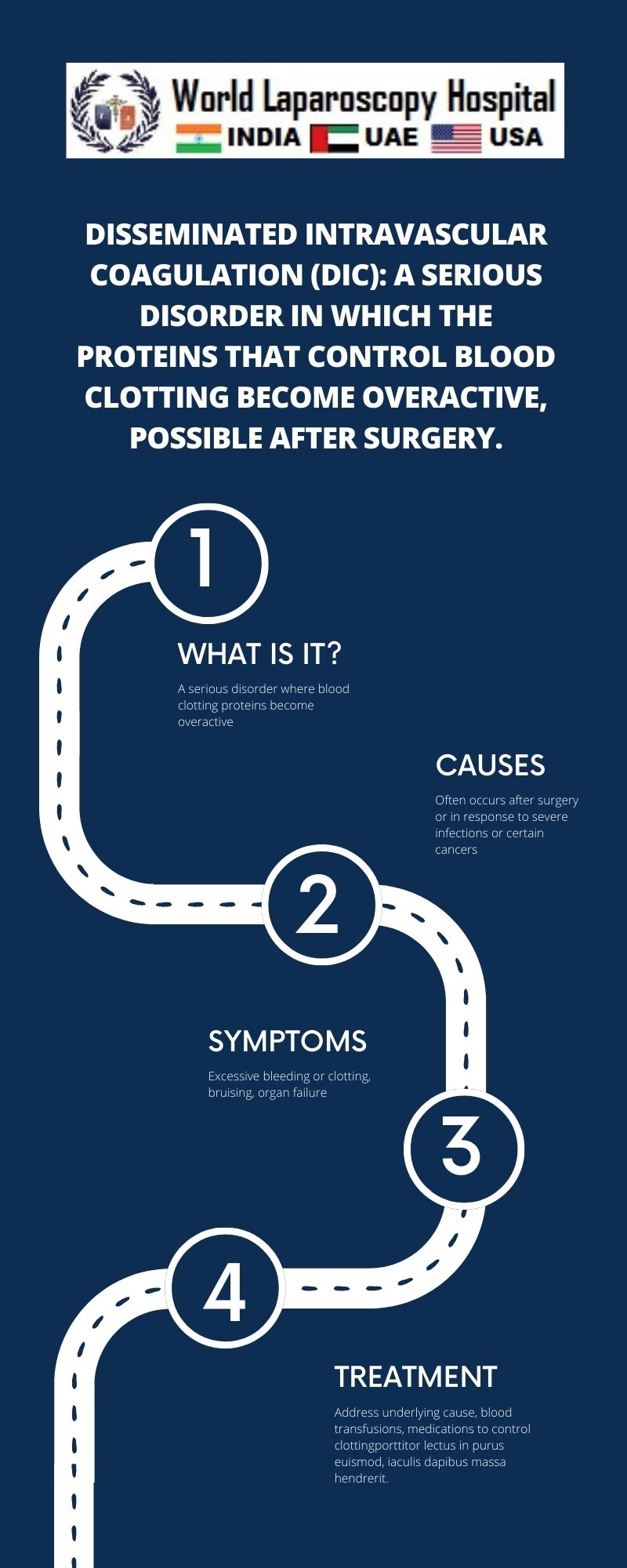
Disseminated intravascular coagulation (DIC): A serious disorder in which the proteins that control blood clotting become overactive, possible after surgery.
Introduction
Disseminated Intravascular Coagulation (DIC) is a complex and serious disorder characterized by the widespread activation of the clotting cascade within the body's blood vessels. It is often triggered by an underlying condition or complication, such as sepsis, trauma, cancer, or major surgery. In DIC, the proteins responsible for controlling blood clotting become overactive, leading to the formation of numerous small blood clots throughout the body's blood vessels. These clots can disrupt normal blood flow and lead to organ damage, bleeding, and other serious complications.
Understanding the Clotting Cascade
To understand DIC, it is important to first understand the normal process of blood clotting, known as the clotting cascade. Blood clotting is a complex process involving a series of steps that occur in response to injury or damage to blood vessels. The clotting cascade is normally tightly regulated to prevent excessive clotting, which can lead to thrombosis (the formation of blood clots within blood vessels) and other complications.
The clotting cascade involves a series of proteins, known as clotting factors, that are activated in a specific sequence. These clotting factors work together to form a stable blood clot. The process begins when a blood vessel is injured, exposing the underlying tissue and triggering the release of chemicals that signal the start of the clotting process.
In DIC, this process becomes dysregulated, leading to the widespread activation of the clotting cascade throughout the body's blood vessels. This excessive activation of clotting factors can deplete the body's supply of clotting factors and platelets, leading to a condition known as consumptive coagulopathy. Consumptive coagulopathy is characterized by the formation of small blood clots throughout the body, which can lead to organ damage and other serious complications.
Causes and Risk Factors
DIC can be triggered by a variety of underlying conditions and complications. Some of the most common causes and risk factors for DIC include:
- Sepsis: DIC is a common complication of severe sepsis, a life-threatening condition caused by a systemic infection.
- Trauma: Severe trauma, such as a major injury or surgery, can trigger DIC due to the release of tissue factors that activate the clotting cascade.
- Cancer: Certain types of cancer, particularly those that involve the blood or bone marrow, can increase the risk of DIC.
- Obstetric complications: DIC can occur as a complication of pregnancy-related conditions, such as placental abruption, preeclampsia, or amniotic fluid embolism.
- Infections: DIC can also occur as a complication of severe infections, such as meningitis or severe pneumonia.
- Liver disease: Liver disease can impair the liver's ability to produce clotting factors, increasing the risk of DIC.
Symptoms and Diagnosis
The symptoms of DIC can vary depending on the underlying cause and the extent of the clotting and bleeding. Some of the most common symptoms of DIC include:
- Excessive bruising or bleeding, such as nosebleeds, bleeding gums, or easy bruising
- Blood in the urine or stool
- Abnormal blood clotting, such as excessive clotting in the veins or arteries
- Organ dysfunction, such as kidney failure or respiratory failure
Diagnosis of DIC can be challenging, as it often occurs in the context of another underlying condition or complication. However, doctors may use a combination of blood tests, such as a complete blood count (CBC), coagulation studies, and tests to measure levels of clotting factors and markers of clotting activation, to diagnose DIC.
Treatment and Management
The treatment of DIC is focused on addressing the underlying cause and managing the complications of the disorder. Treatment may include:
- Treating the underlying condition or complication, such as sepsis or trauma
- Providing supportive care, such as blood transfusions to replace depleted clotting factors and platelets
- Administering medications to help regulate the clotting cascade, such as anticoagulants or medications to promote fibrinolysis (the breakdown of blood clots)
- Managing complications, such as organ dysfunction or bleeding
The prognosis for DIC can vary depending on the underlying cause and the extent of organ damage. However, early recognition and treatment of DIC are crucial for improving outcomes and reducing the risk of complications.
Prevention
Preventing DIC often involves reducing the risk of the underlying conditions or complications that can trigger the disorder. This may include:
- Practicing good hygiene to reduce the risk of infections
- Seeking prompt medical attention for severe injuries or trauma
- Managing underlying medical conditions, such as cancer or liver disease, to reduce the risk of complications
Conclusion
Disseminated Intravascular Coagulation (DIC) is a serious and complex disorder characterized by the widespread activation of the clotting cascade within the body's blood vessels. It is often triggered by an underlying condition or complication, such as sepsis, trauma, cancer, or major surgery. DIC can lead to the formation of numerous small blood clots throughout the body, which can disrupt normal blood flow and lead to organ damage, bleeding, and other serious complications. Early recognition and treatment of DIC are crucial for improving outcomes and reducing the risk of complications. Prevention of DIC often involves reducing the risk of the underlying conditions or complications that can trigger the disorder.