Introduction
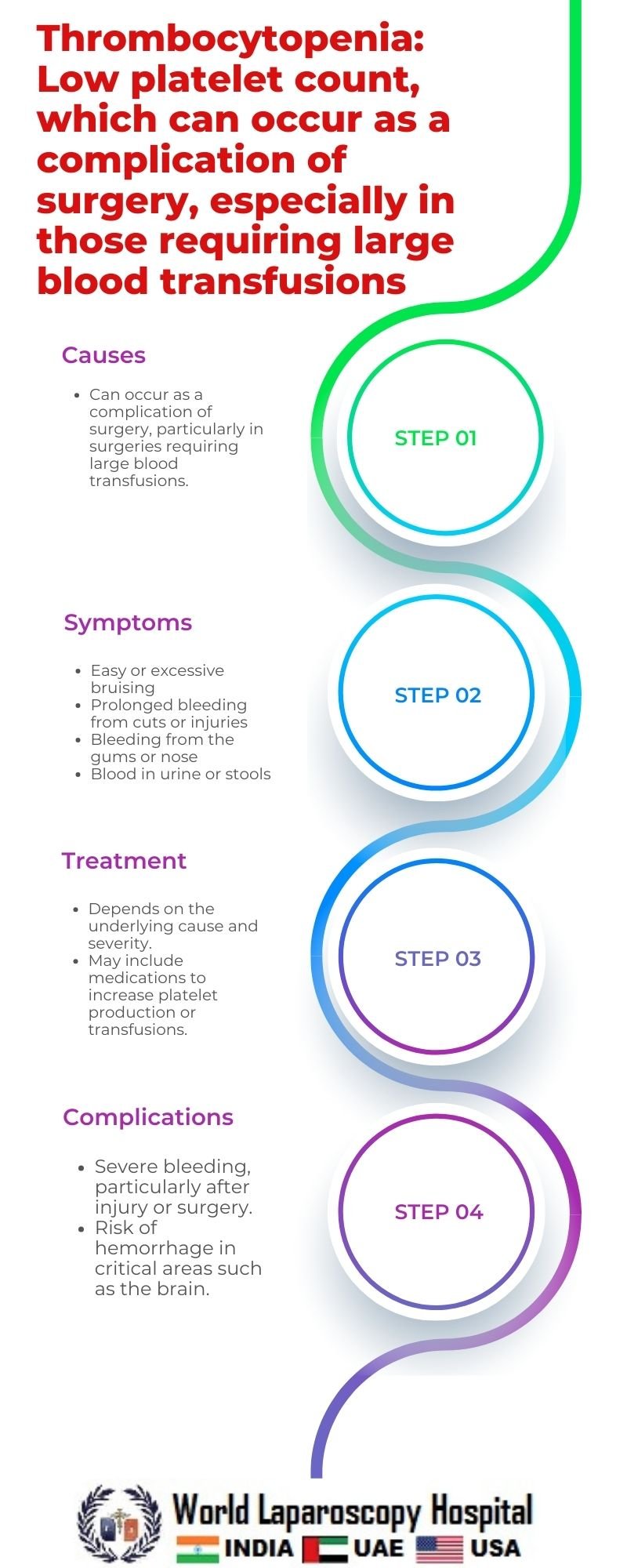
Thrombocytopenia, characterized by a low platelet count, is a condition that can occur as a complication of surgery, particularly in patients requiring large blood transfusions. Platelets are essential for blood clotting, and a low platelet count can lead to increased risk of bleeding, which can be a serious concern during and after surgery. Understanding the causes, symptoms, and management of thrombocytopenia in surgical settings is crucial for healthcare professionals to provide optimal care to their patients.
Causes of Thrombocytopenia in Surgery
Thrombocytopenia in surgical patients can have various causes, including pre-existing conditions such as immune thrombocytopenia (ITP), myelodysplastic syndrome (MDS), or leukemia. However, in the context of surgery, the most common cause is perioperative blood loss and dilutional thrombocytopenia due to large-volume blood transfusions. Surgery can lead to significant blood loss, and patients may require transfusion of packed red blood cells (PRBCs) and other blood products to maintain hemostasis. This can dilute the platelet count and contribute to thrombocytopenia.
Other causes of thrombocytopenia in surgical patients include sepsis, medications such as heparin, and disseminated intravascular coagulation (DIC), which can occur as a complication of surgery or underlying conditions. It is essential for healthcare providers to evaluate the underlying cause of thrombocytopenia to determine the most appropriate management strategy.
Symptoms and Diagnosis
The symptoms of thrombocytopenia can vary depending on the severity of the condition. Mild thrombocytopenia may not cause any symptoms, while severe thrombocytopenia can lead to excessive bleeding, easy bruising, and petechiae (small red or purple spots on the skin). In surgical patients, symptoms of thrombocytopenia may be masked by postoperative pain and other surgical complications, highlighting the importance of routine monitoring of platelet counts.
Diagnosis of thrombocytopenia in surgical patients is typically based on a complete blood count (CBC) with differential, which includes a platelet count. Additional tests, such as peripheral blood smear, bone marrow aspiration, and specific blood tests to detect underlying causes, may be necessary in certain cases. Differential diagnosis should also include ruling out pseudothrombocytopenia, a condition where platelets clump together in a blood sample, leading to a falsely low platelet count.
Management of Thrombocytopenia in Surgery
The management of thrombocytopenia in surgical patients depends on the underlying cause and the severity of the condition. In cases where thrombocytopenia is due to perioperative blood loss and dilutional thrombocytopenia, transfusion of platelets may be necessary to maintain an adequate platelet count and prevent bleeding complications. Platelet transfusions should be guided by the patient's clinical condition, platelet count, and risk of bleeding.
In patients with immune thrombocytopenia (ITP) or other autoimmune conditions causing thrombocytopenia, corticosteroids, intravenous immunoglobulin (IVIG), and immunosuppressive agents may be used to increase platelet counts. In some cases, splenectomy may be considered as a treatment option to remove the site of platelet destruction.
Prevention of Thrombocytopenia in Surgery
Preventing thrombocytopenia in surgical patients involves careful management of perioperative blood loss and judicious use of blood transfusions. Preoperative optimization of platelet counts and coagulation parameters, when possible, can help minimize the risk of thrombocytopenia during surgery. In cases where large-volume blood transfusions are anticipated, the use of cell salvage techniques and blood conservation strategies can reduce the need for allogeneic blood products and the risk of dilutional thrombocytopenia.
Conclusion
Thrombocytopenia is a common complication of surgery, especially in patients requiring large blood transfusions. Understanding the causes, symptoms, and management of thrombocytopenia in surgical settings is crucial for healthcare providers to provide optimal care to their patients. By identifying and managing thrombocytopenia early, healthcare providers can reduce the risk of bleeding complications and improve patient outcomes.