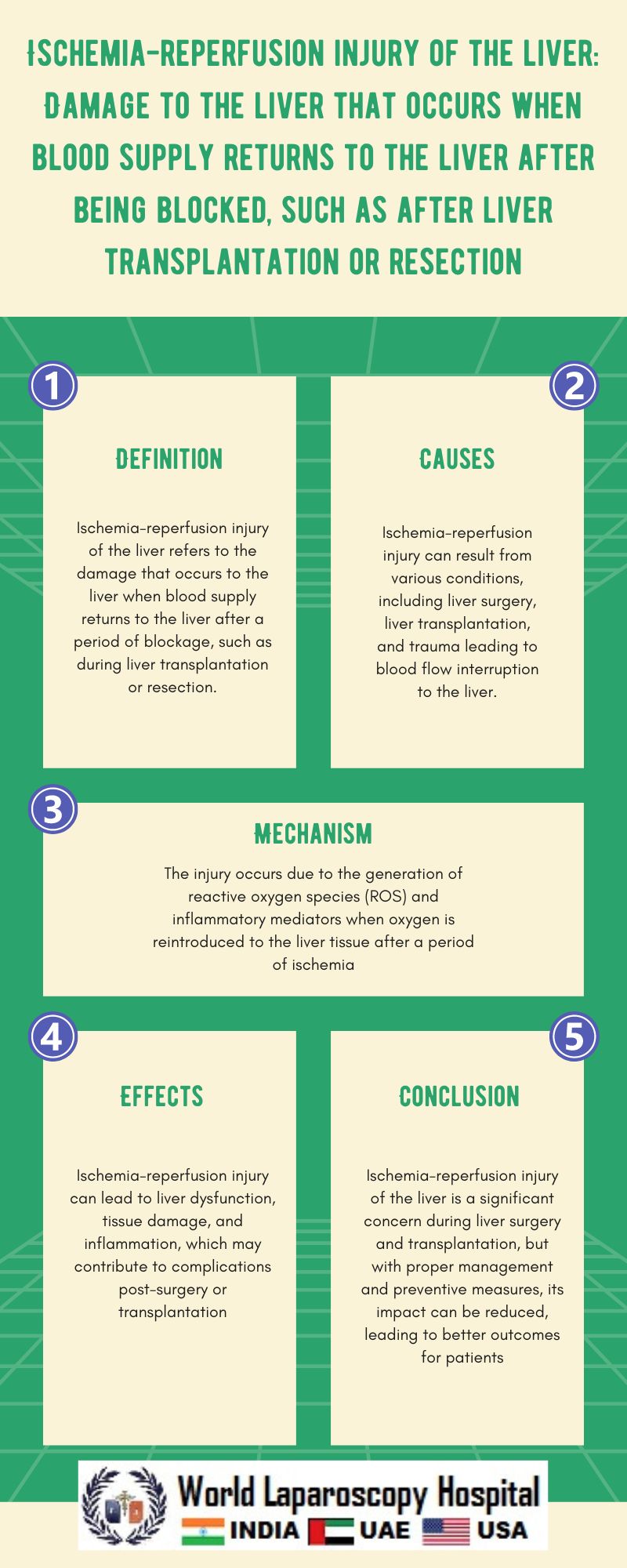
Ischemia-reperfusion injury (IRI) of the liver is a major concern in clinical settings such as liver transplantation, hepatic resection, and trauma. IRI occurs when the blood supply to the liver is temporarily interrupted, leading to tissue damage and dysfunction. The subsequent restoration of blood flow, known as reperfusion, further exacerbates the injury, resulting in a cascade of inflammatory and oxidative stress responses. This article explores the mechanisms underlying IRI of the liver and discusses current strategies for minimizing its impact in clinical practice.
Mechanisms of Ischemia-Reperfusion Injury
The pathophysiology of IRI of the liver is complex and involves multiple interconnected pathways. The initial phase of ischemia leads to a depletion of oxygen and nutrients, resulting in cellular dysfunction and metabolic alterations. During this phase, the liver undergoes a series of changes, including the activation of inflammatory mediators, the release of reactive oxygen species (ROS), and the induction of cell death pathways.
Reperfusion exacerbates the injury by triggering an inflammatory response characterized by the infiltration of immune cells, such as neutrophils and macrophages, into the liver. These immune cells release pro-inflammatory cytokines and ROS, further damaging hepatocytes and promoting tissue injury. Additionally, reperfusion leads to the formation of mitochondrial permeability transition pores (MPTPs), which disrupt mitochondrial function and contribute to cell death.
Clinical Implications of Ischemia-Reperfusion Injury
IRI of the liver has significant clinical implications, particularly in the context of liver transplantation and hepatic resection. In liver transplantation, IRI can lead to primary graft dysfunction, delayed graft function, and early allograft dysfunction, all of which are associated with increased morbidity and mortality. Similarly, in hepatic resection, IRI can contribute to postoperative liver failure and complications, impacting patient outcomes.
Strategies for Minimizing Ischemia-Reperfusion Injury
Several strategies have been proposed to minimize the impact of IRI in clinical practice. Preconditioning, both ischemic and pharmacological, has been shown to induce a protective effect against IRI by activating endogenous protective pathways and reducing oxidative stress. Similarly, the use of anti-inflammatory agents, antioxidants, and mitochondrial protectants has shown promise in reducing IRI-induced liver damage.
Conclusion
Ischemia-reperfusion injury of the liver is a complex process that occurs during various clinical scenarios, such as liver transplantation and hepatic resection. The mechanisms underlying IRI involve a cascade of inflammatory and oxidative stress responses that can significantly impact patient outcomes. Understanding these mechanisms is crucial for developing strategies to minimize the impact of IRI and improve clinical outcomes in patients undergoing liver surgery or transplantation.