Introduction:
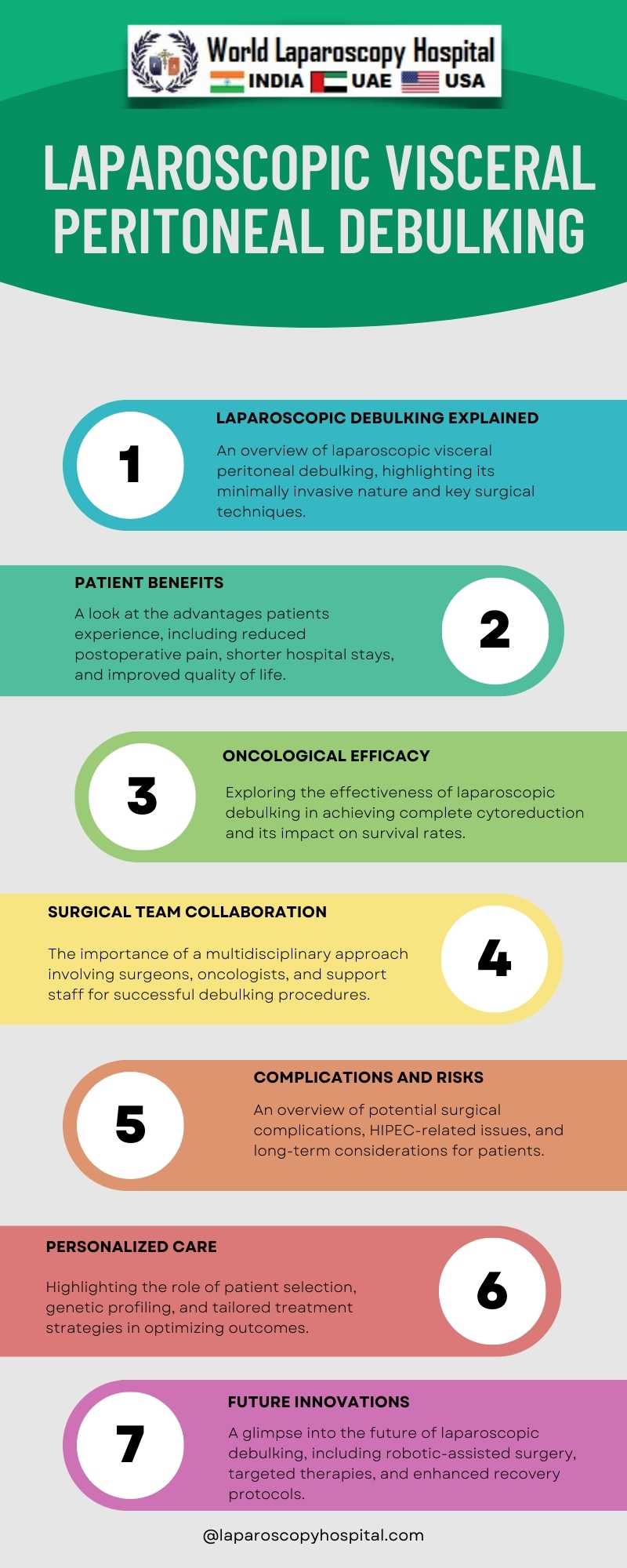
In the field of surgical oncology, laparoscopic visceral peritoneal debulking has emerged as a revolutionary technique in the management of peritoneal surface malignancies. This minimally invasive approach offers the promise of not only achieving excellent oncological outcomes but also significantly enhancing patient recovery and quality of life. In this article, we delve into the world of laparoscopic visceral peritoneal debulking, exploring its evolution, techniques, efficacy, and the crucial aspect of bridging the gap between clinical success and the patient's journey to recovery.
I. Historical Perspective
To appreciate the significance of laparoscopic visceral peritoneal debulking, we must first take a step back in time. Traditional open surgeries for peritoneal surface malignancies often involved extensive incisions, prolonged hospital stays, and a challenging recovery period. The advent of laparoscopy revolutionized this landscape by introducing minimally invasive techniques. This section explores the historical context and the milestones that paved the way for laparoscopic approaches.
II. Techniques and Surgical Innovations
A. Exploring the Laparoscopic Toolbox
1. Trocar Placement and Port Selection
2. Carbon Dioxide Insufflation
3. Optics and Visualization
B. Peritoneal Surface Malignancies
1. Ovarian Cancer
2. Colorectal Cancer
3. Appendiceal Neoplasms
4. Mesothelioma
5. Pseudomyxoma Peritonei
C. Cytoreductive Surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC)
1. Patient Selection
2. The Role of CRS in Debulking
3. HIPEC: Enhancing the Therapeutic Effect
III. Bridging Efficacy and Outcomes
A. Oncological Efficacy
1. Complete Cytoreduction: The Gold Standard
2. Survival Benefits and Prognostic Factors
3. Managing Recurrence
B. Quality of Life
1. Reduced Postoperative Pain
2. Faster Recovery and Shorter Hospital Stays
3. Improved Cosmesis
4. Preservation of Function
C. Patient-Reported Outcomes
1. Physical and Emotional Well-being
2. Coping with Long-term Effects
3. Survivorship and Follow-up Care
IV. Challenges and Considerations
A. Learning Curve
1. Training and Skill Acquisition
2. Team Collaboration
B. Patient Selection
1. Disease Extent and Comorbidities
2. Age and Performance Status
C. Complications and Adverse Events
1. Surgical Complications
2. HIPEC-Related Issues
3. Long-term Consequences
V. Case Studies and Clinical Insights
A. Case 1: Ovarian Cancer
1. Surgical Approach and Outcome
2. Patient Recovery Journey
B. Case 2: Colorectal Cancer
1. Challenging Anatomy and Surgical Solutions
2. Rehabilitation and Postoperative Support
C. Case 3: Pseudomyxoma Peritonei
1. Multidisciplinary Care
2. Long-term Follow-up and Survivorship
VI. Future Directions and Innovations
A. Robotic-Assisted Laparoscopy
1. Advantages and Potential
2. Current Research and Developments
B. Personalized Medicine and Targeted Therapies
1. Tailoring Treatment Strategies
2. Genetic Profiling and Predictive Markers
C. Enhanced Recovery After Surgery (ERAS) Protocols
1. Holistic Patient Care
2. Multimodal Pain Management
Conclusion:
Laparoscopic visceral peritoneal debulking represents a remarkable convergence of surgical skill, technological advancement, and patient-centered care. It offers the prospect of not only achieving optimal oncological outcomes but also bridging the gap between efficacy and patient recovery. As this field continues to evolve, it is imperative that surgeons, researchers, and healthcare providers collaborate to refine techniques, enhance patient selection, and further improve the quality of life for individuals facing peritoneal surface malignancies. By embracing innovation, emphasizing personalized care, and sharing clinical insights, we can continue to advance the frontiers of laparoscopic visceral peritoneal debulking and provide hope to patients and their families.