Introduction
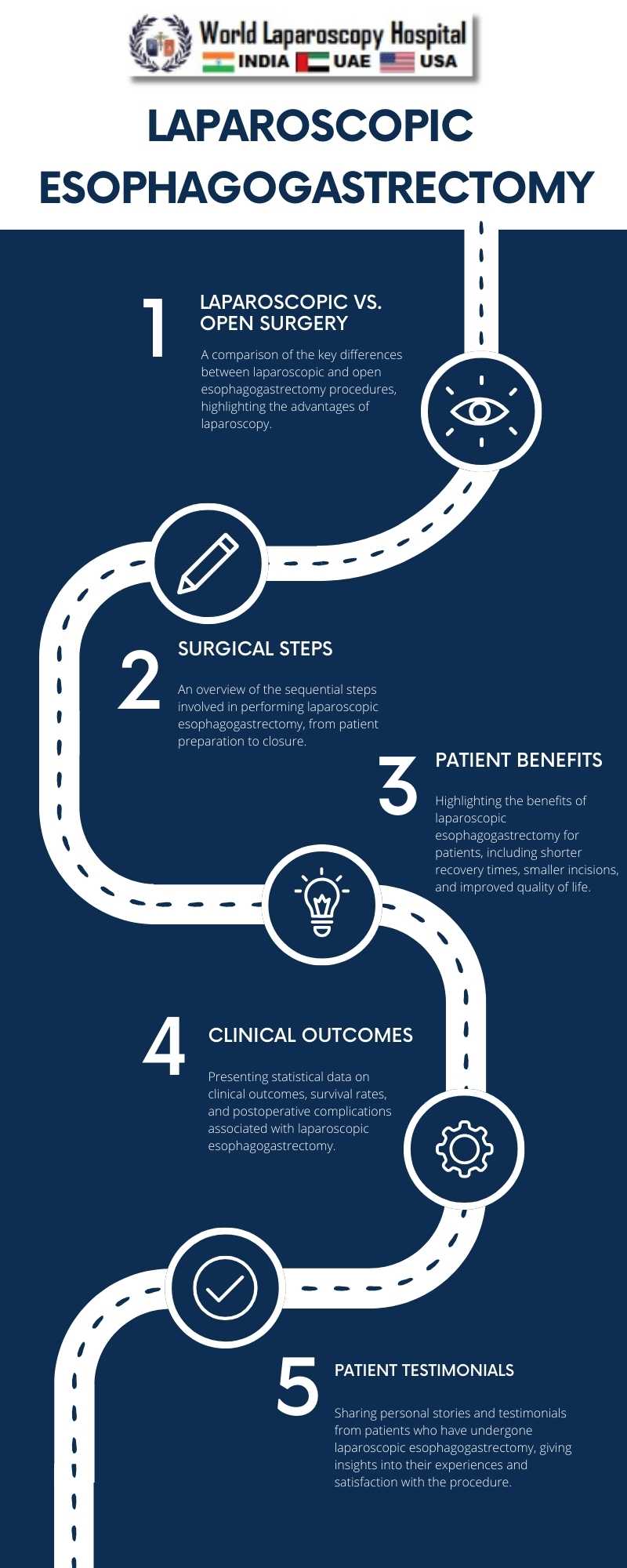
The field of surgery has witnessed remarkable advancements in recent decades, particularly in the realm of minimally invasive techniques. Laparoscopic surgery, often referred to as "keyhole surgery," has revolutionized the way various surgical procedures are performed. One such procedure that has benefited immensely from this innovation is Laparoscopic Esophagogastrectomy, which has emerged as a key approach to surgery involving the gastroesophageal junction. In this article, we delve into the intricacies of Laparoscopic Esophagogastrectomy, exploring its evolution, techniques, benefits, and the impact it has had on patients' lives.
I. Historical Evolution
To truly appreciate the significance of Laparoscopic Esophagogastrectomy, we must first trace its historical evolution. Traditional open surgeries for conditions affecting the gastroesophageal junction were often associated with significant morbidity and prolonged recovery periods. The introduction of laparoscopy in the late 20th century marked a pivotal moment in surgical history. Surgeons began exploring its application in procedures involving the esophagus and stomach.
II. Laparoscopic Techniques
Laparoscopic Esophagogastrectomy involves the use of minimally invasive techniques to remove a portion of the esophagus and stomach, typically to treat conditions such as esophageal cancer or severe gastroesophageal reflux disease (GERD). This section of the article will delve into the key techniques and steps involved in performing this surgery, including:
1. Patient Preparation: Pre-operative evaluation and patient selection are critical for successful laparoscopic esophagogastrectomy.
2. Anesthesia and Trocar Placement: The importance of anesthesia and the strategic placement of trocars for optimal visualization and instrument access.
3. Mobilization of the Stomach and Esophagus: Techniques for safely mobilizing the stomach and esophagus from surrounding structures.
4. Resection and Reconstruction: The actual resection of the affected segment and various methods of reconstruction, including the creation of an esophagogastric anastomosis.
5. Lymphadenectomy: The role of lymphadenectomy in cancer cases and the meticulous dissection of lymph nodes.
6. Hemostasis and Closure: Ensuring adequate hemostasis and closure of incisions.
III. Advantages of Laparoscopic Esophagogastrectomy
The advantages of laparoscopic esophagogastrectomy over traditional open surgery cannot be overstated. This section explores the numerous benefits, including:
1. Minimized Surgical Trauma: Reduced tissue damage, leading to less postoperative pain and faster recovery.
2. Smaller Incisions: Improved cosmetic outcomes and reduced risk of wound complications.
3. Shorter Hospital Stay: Patients often spend less time in the hospital, resulting in cost savings.
4. Quicker Return to Normal Function: Patients can resume normal activities sooner, enhancing their quality of life.
5. Lower Risk of Complications: Reduced risk of infection, herniation, and other postoperative complications.
IV. Clinical Outcomes and Survival Rates
A critical aspect of any surgical procedure is its impact on patient outcomes. This section discusses the clinical outcomes and survival rates associated with laparoscopic esophagogastrectomy, with a focus on its effectiveness in treating esophageal cancer and GERD-related conditions. Statistical data and case studies will be presented to illustrate the procedure's success in improving patient prognosis.
V. Patient Perspectives
Incorporating the patient's perspective is essential to understand the true impact of laparoscopic esophagogastrectomy. This section features personal stories and testimonials from patients who have undergone the procedure. These accounts shed light on their experiences, challenges, and postoperative quality of life, providing valuable insights for both healthcare providers and prospective patients.
VI. Future Directions and Challenges
The article concludes by exploring the future directions of laparoscopic esophagogastrectomy, including ongoing research, technological advancements, and potential innovations. Additionally, it addresses the challenges that the surgical community must overcome to further improve the procedure's safety and effectiveness.
Conclusion
Laparoscopic Esophagogastrectomy has transformed the landscape of gastroesophageal junction surgery, offering patients a less invasive and more efficient approach to treatment. This article has provided an in-depth exploration of the procedure's historical evolution, techniques, advantages, clinical outcomes, patient perspectives, and future prospects. As the surgical field continues to evolve, laparoscopic esophagogastrectomy stands as a shining example of how innovation can lead to improved patient care and outcomes in the world of surgery.