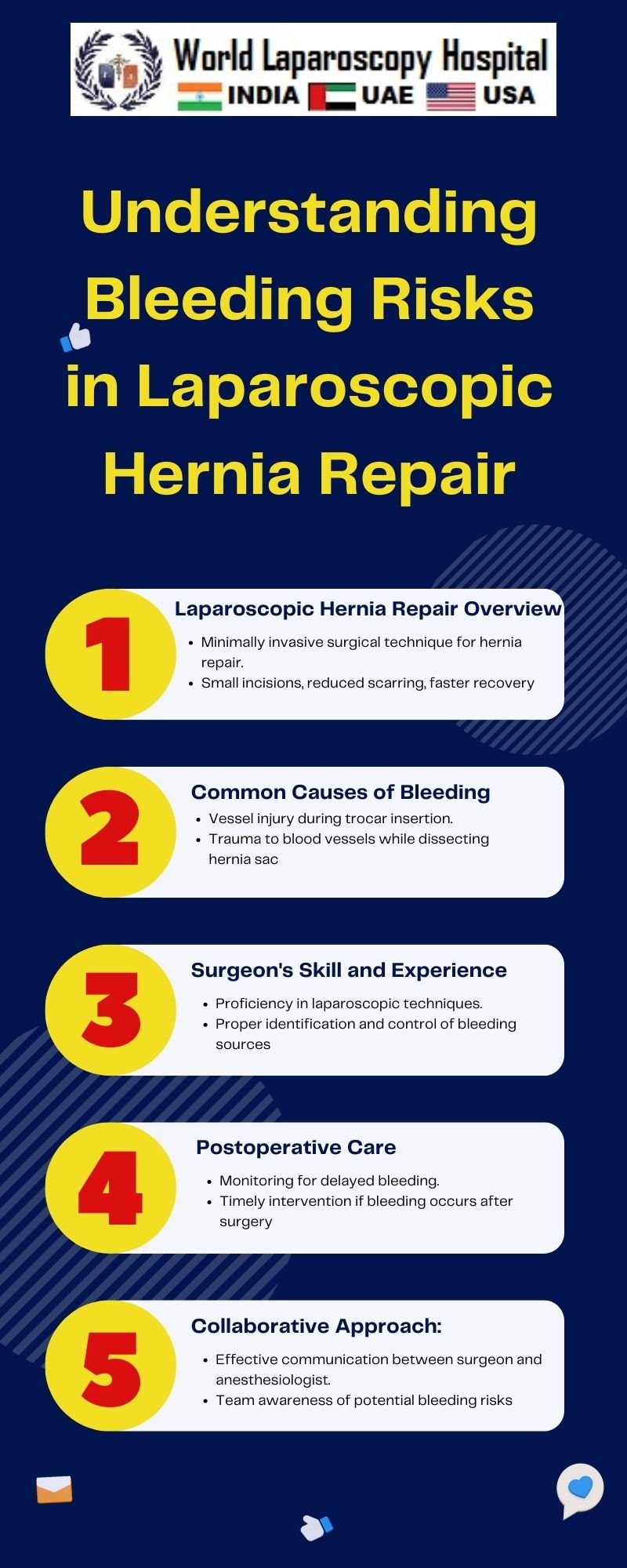
Understanding Bleeding Risks in Laparoscopic Hernia Repair
Introduction
Laparoscopic hernia repair has emerged as a revolutionary technique, offering patients a minimally invasive alternative to traditional open surgeries. While hailed for its benefits, such as reduced postoperative pain and quicker recovery times, it is crucial to delve into the nuances of this procedure to fully comprehend potential complications. One such concern that demands careful consideration is bleeding risks associated with laparoscopic hernia repair.
Laparoscopic Hernia Repair: An Overview
Before diving into the intricacies of bleeding risks, let's first establish a foundational understanding of laparoscopic hernia repair. This modern approach involves using small incisions through which a laparoscope and specialized instruments are inserted. The surgeon navigates these instruments to place a mesh or patch over the hernia, reinforcing the weakened area and preventing a recurrence.
Benefits of Laparoscopic Hernia Repair
-
Minimally Invasive Nature Laparoscopic hernia repair boasts the advantage of minimal invasiveness, contributing to reduced postoperative pain, shorter hospital stays, and faster recovery times compared to traditional open surgeries.
-
Improved Cosmesis Smaller incisions result in less scarring, providing patients with a more aesthetically pleasing outcome. This cosmetic benefit is particularly relevant in an era where patients often prioritize both the efficacy of the procedure and its impact on appearance.
Bleeding Risks in Laparoscopic Hernia Repair
Despite the advantages, it is essential to acknowledge that no surgical procedure is without risks. Bleeding, in particular, can pose a challenge during laparoscopic hernia repair. Understanding the potential sources and mitigating factors is crucial for both surgeons and patients.
-
Vascular Injury One of the primary sources of bleeding risk in laparoscopic hernia repair is inadvertent vascular injury. The proximity of blood vessels to the hernia site increases the likelihood of accidental trauma during the insertion and manipulation of instruments. Identifying these vessels promptly and employing meticulous surgical techniques are critical to reducing the risk of vascular injury.
-
Trocar Placement The strategic placement of trocars, the sleeves through which instruments are inserted, is paramount in minimizing bleeding risks. Poorly positioned trocars can damage blood vessels, leading to bleeding complications. Surgeons must exercise precision in trocar placement and constantly reassess their positioning throughout the procedure.
Mitigating Bleeding Risks: A Comprehensive Approach
-
Preoperative Assessment Thorough preoperative assessment is the foundation for a successful laparoscopic hernia repair. Surgeons must diligently review patients' medical histories, paying close attention to factors such as coagulation disorders, medication use, and any previous abdominal surgeries. A comprehensive understanding of these elements enables surgeons to tailor their approach and implement appropriate precautions.
-
Hemostasis Techniques In the event of bleeding during laparoscopic hernia repair, effective hemostasis techniques are essential. Surgeons must be adept at promptly identifying the source of bleeding and employing various methods to achieve hemostasis, including electrocautery, clips, and hemostatic agents.
-
Use of Hemostatic Agents Advancements in surgical technology have introduced hemostatic agents that can be invaluable in managing bleeding risks. These agents, such as topical hemostatic patches or powders, can be applied directly to the bleeding site to expedite clotting and minimize blood loss.
Postoperative Care and Monitoring
-
Vigilant Observation Postoperative monitoring is crucial to detect any signs of bleeding or complications promptly. Vigilant observation, coupled with regular follow-up appointments, allows surgeons to intervene promptly if issues arise.
-
Patient Education Empowering patients with knowledge about potential bleeding risks and the signs of complications is equally important. Providing clear postoperative care instructions and encouraging patients to report any unusual symptoms fosters a collaborative approach to recovery.
Conclusion
In conclusion, while laparoscopic hernia repair stands as a remarkable advancement in surgical techniques, the potential for bleeding complications necessitates a nuanced understanding and proactive approach. Surgeons must navigate the intricate landscape of blood vessels, employ meticulous techniques, and leverage technological advancements to minimize bleeding risks. Patient education and thorough preoperative assessments further contribute to a comprehensive strategy in ensuring successful outcomes in laparoscopic hernia repair. As the field continues to evolve, ongoing research and advancements in surgical practices will undoubtedly enhance our ability to navigate and mitigate bleeding risks effectively.