In the realm of medicine, there exist a myriad of conditions that can challenge even the most seasoned healthcare professionals. One such condition, Neuroleptic Malignant Syndrome (NMS), stands out as a rare but potentially life-threatening reaction to neuroleptic medications. While typically associated with psychiatric care, NMS can also rear its head in the surgical setting, adding a layer of complexity to patient management.
Understanding Neuroleptic Malignant Syndrome
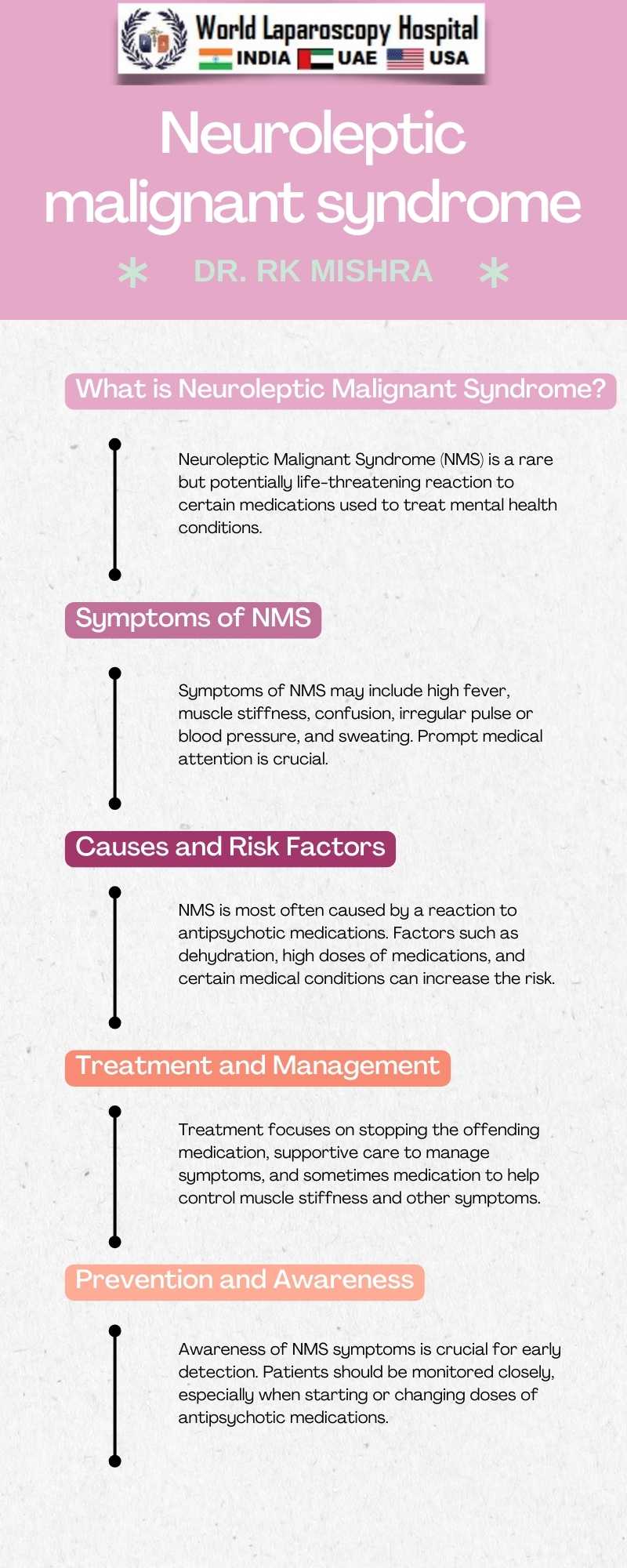
Neuroleptic Malignant Syndrome is a rare, idiosyncratic reaction to neuroleptic medications, characterized by a spectrum of symptoms ranging from muscle rigidity, fever, altered mental status, and autonomic dysfunction. Although the exact pathophysiology remains unclear, it is believed to involve central dopamine blockade leading to a cascade of events culminating in the syndrome's clinical manifestations.
NMS in the Surgical Context
While NMS is more commonly encountered in psychiatric patients, its occurrence in surgical patients, though rare, poses unique challenges. Patients undergoing surgery may receive neuroleptic medications for various reasons, such as preoperative sedation, management of delirium, or treatment of psychiatric conditions. The use of these medications in the perioperative period can potentially precipitate NMS, especially in susceptible individuals.
Clinical Presentation and Diagnosis
The clinical presentation of NMS can mimic other conditions such as malignant hyperthermia, serotonin syndrome, and sepsis, making its diagnosis challenging. Suspicion should be high in patients receiving neuroleptic medications who develop muscle rigidity, hyperthermia, and altered mental status. Laboratory investigations may reveal elevated creatine kinase levels, leukocytosis, and electrolyte abnormalities, supporting the diagnosis.
Management and Treatment Considerations
The cornerstone of NMS management revolves around early recognition and prompt discontinuation of the offending neuroleptic medication. Supportive care, including hydration, temperature control, and monitoring for complications such as rhabdomyolysis and renal failure, is paramount. In severe cases, pharmacological interventions such as dantrolene and bromocriptine may be considered to mitigate symptoms.
Prevention and Risk Mitigation
Preventing NMS in the surgical setting involves careful consideration of the risks and benefits of neuroleptic medication use. Alternative strategies for sedation and management of psychiatric symptoms should be explored whenever possible. Additionally, close monitoring of patients receiving neuroleptics, especially those with predisposing factors such as dehydration, agitation, and polypharmacy, can help mitigate the risk of NMS development.
Conclusion
In conclusion, Neuroleptic Malignant Syndrome is a rare but potentially life-threatening condition that can occur in the surgical setting. Healthcare professionals, including surgeons, anesthesiologists, and nurses, should be aware of its clinical presentation, diagnostic criteria, and management principles to ensure timely recognition and intervention. By maintaining a high index of suspicion and implementing preventive measures, the impact of NMS on patient outcomes can be minimized, ensuring safe and effective perioperative care.
This blog post aims to raise awareness about NMS in the surgical setting, highlighting its clinical significance and management strategies. As with any medical condition, early recognition and appropriate intervention are crucial in ensuring favorable patient outcomes.