Visual Guide: Laparoscopic Repair of Left-Sided Complete Indirect Inguinal Hernia
Add to
Share
1,313 views
Report
1 year ago
Description
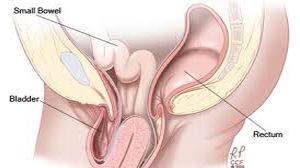
Introduction: In recent years, surgical techniques have undergone significant advancements, leading to safer and more efficient procedures with reduced recovery times for patients. One such innovation is the skin-to-skin approach for laparoscopic repair of left-sided complete indirect inguinal hernias. This method represents a departure from traditional techniques, offering numerous benefits to both surgeons and patients. In this comprehensive discussion, we will delve into the intricacies of this surgical approach, exploring its advantages, techniques, and outcomes. Understanding Left-Sided Complete Indirect Inguinal Hernia: Before delving into the surgical technique, it is essential to understand the condition being addressed. A left-sided complete indirect inguinal hernia occurs when abdominal contents protrude through the inguinal canal, traveling along the spermatic cord in males or the round ligament in females. This type of hernia is characterized by its complete displacement into the inguinal canal, posing risks of complications such as bowel obstruction or strangulation if left untreated. Traditional Surgical Approaches: Historically, the surgical repair of inguinal hernias involved open procedures, which required a larger incision and longer recovery times. With advancements in minimally invasive techniques, laparoscopic approaches emerged as a preferred option due to their reduced postoperative pain, shorter hospital stays, and quicker return to normal activities. However, traditional laparoscopic methods still necessitated multiple incisions, resulting in additional scarring and potential complications. The Skin-to-Skin Laparoscopic Approach: The skin-to-skin laparoscopic repair of left-sided complete indirect inguinal hernias represents a refinement of existing techniques, aiming to minimize invasiveness and optimize patient outcomes. Unlike traditional methods that require separate incisions for trocars and ports, this approach involves a single small incision at the umbilicus, through which both the camera and working instruments are inserted. Key Steps of the Procedure: 1. Patient Preparation: The patient is placed under general anesthesia, and the surgical site is prepped and draped in a sterile fashion. 2. Incision and Trocar Placement: A small incision is made at the umbilicus, and a trocar is inserted to create a port for the laparoscope. 3. Insufflation and Visualization: Carbon dioxide gas is insufflated into the abdomen to create a working space, and the laparoscope is inserted to visualize the hernia defect and surrounding anatomy. 4. Instrument Insertion: Additional trocars are inserted through the same umbilical incision to accommodate working instruments, such as graspers and dissectors. 5. Reduction and Repair: The hernia sac is dissected and reduced back into the abdominal cavity, and the defect is repaired using mesh or sutures to reinforce the weakened area. 6. Closure: Once the repair is complete, the instruments are removed, and the umbilical incision is closed with sutures or adhesive strips. Advantages of Skin-to-Skin Laparoscopic Repair: 1. Reduced Incisional Trauma: By utilizing a single incision at the umbilicus, the skin-to-skin approach minimizes tissue trauma and scarring, resulting in improved cosmetic outcomes. 2. Decreased Postoperative Pain: With fewer incisions, patients experience less postoperative pain and require lower doses of analgesics, facilitating a quicker recovery. 3. Enhanced Cosmetic Outcome: The single umbilical incision is less noticeable than multiple incisions, leading to improved patient satisfaction with the cosmetic result. 4. Shorter Hospital Stay: Patients undergoing skin-to-skin laparoscopic repair typically experience shorter hospital stays compared to those undergoing traditional laparoscopic or open procedures. 5. Quicker Return to Normal Activities: The minimally invasive nature of the procedure allows patients to resume normal activities sooner, leading to a faster overall recovery time. Clinical Outcomes and Patient Satisfaction: Studies evaluating the skin-to-skin laparoscopic approach have reported favorable clinical outcomes, including low rates of recurrence and complications. Furthermore, patients consistently express high levels of satisfaction with the cosmetic result and their overall experience with the procedure. These findings underscore the effectiveness and patient-centered nature of this innovative surgical technique. Conclusion: The skin-to-skin laparoscopic repair of left-sided complete indirect inguinal hernias represents a significant advancement in surgical technique, offering numerous benefits over traditional approaches. By minimizing incisional trauma, reducing postoperative pain, and optimizing cosmetic outcomes, this approach enhances patient satisfaction while maintaining excellent clinical results. As minimally invasive techniques continue to evolve, the skin-to-skin approach stands out as a promising option for hernia repair, paving the way for improved outcomes and experiences for patients undergoing surgical treatment.

Similar Videos