TASK ANALYSIS FOR LAPAROSCOPIC SALPINGOTOMY
Dr. Anjali Gupta M.S (OBS AND GYNE) AJMER RAJASTHAN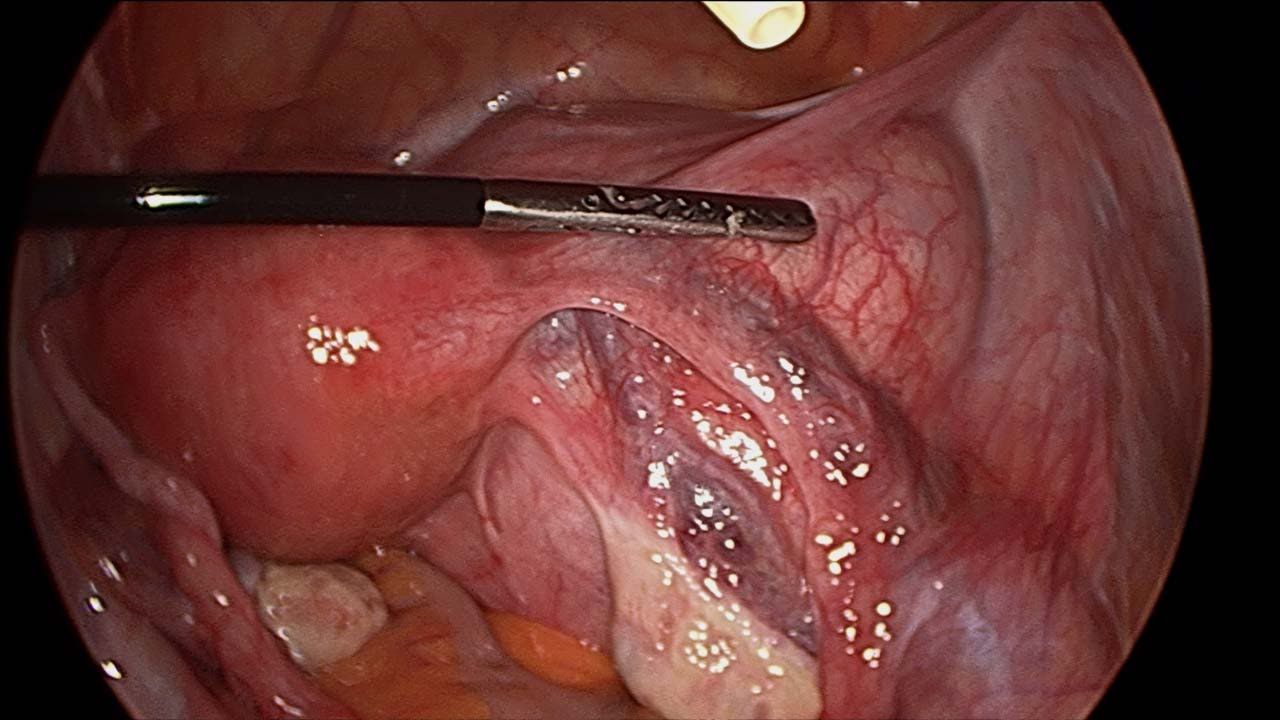
Preoperative preparations:
1. Blood investigations and Pre-Anesthetic check-up
2. Crossmatch
3. Informed consent
4. Preoperative Antibiotics
5. Surgical team: Surgeon, Anesthetist, Assistant, Scrubbed nurse
Equipment and Laparoscopy Tower:
1. Monitor (Desirable 26” HD)
2. Light Source and Camera Control Unit (Desirable – LED light source and 3 Chip HD Camera)
3. Insufflators and CO2 Gas Cylinder
4. Electro Surgical Unit (Desirable – High-Frequency Generator)
5. Select Pre-set Pressure (Ideal 12 to 15mmHg)
6. Video Recorder & Printer
7. Suction Irrigation system
8. Veress' needle – 12 cm length
9. Ports: One 10mm reusable port, two 5mm ancillary ports
Laparoscopic set :
. Maryland.
. Laparoscopy Aspiration Needle
. Laparoscopic scissors
. Atraumatic grasping forceps
. Tritome
. Suction Irrigation 5 mm
. Syringe and Normal Saline (10ml)
. Vasopressin 5 unit diluted in 20 ml of saline.
. Sterile dressing
Position of the patient: Supine position
Position of the surgical team and equipment:
1. The surgeon should stand on the left side of the patient and the distance from the screen is 5 times
diagonal length of the screen which is placed opposite and in front of the surgeon.
2. Assistant on the right of the surgeon.
3. Scrub nurse on the left of the surgeon.
4. Anesthetist in the usual position on the head end.
Procedure:
Optical port site inferior Crease of Umbilicus (Scandinavian method)
1. Hold umbilicus with Allis forceps on either side to Evert the inferior crease of umbilicus
2. Make a stab incision of 2mm with No. 11 surgical blade
3. Check Veress Needle for its spring action and patency
4. Lift up the abdominal wall below the umbilicus and assess its full thickness,
5. Veress Needle is held like a dart at a distance of 4 cm plus the thickness of the abdominal wall from its
distal end.
6. Insertion of veress needle through the incision site in a manner that the veress needle makes an
angle of 90’ with the abdominal wall and an angle of 45’ with the body of patient, pointing towards
the anus.
8. Insertion is achieved with two audible clicks; first of the Rectus Sheath and second of the
Peritoneum
9. Release the Allis forceps from the Abdominal wall
10. Hold the Veress Needle at an angle of 45’ making sure that no further length of needle is
advanced.
11. Confirm the intraperitoneal placement of the veress needle by ASPIRATION TEST,
IRRIGATION TEST and HANGING DROP TEST
12. Ensure that the Gas tubing is attached to the Insufflator and the Insufflator is switched ON. This
will remove air from the Gas tubing and fill the gas tubing till its tip with CO2 gas.
13. Confirm Pre-Set Pressure to 15mmHg on the Insufflator
14. Attach the gas tubing to the veress needle and start the flow of CO2gas at 1 liter per minute
15. Confirm obliteration of liver dullness and generalized distension of abdominal wall
16. Keep watch on patient’s vital parameters and EtCO2 readings during insufflation
18. The total amount of gas and actual pressure should rise in a linear fashion.
19. When actual pressure has reached pre-set pressure and amount of gas used might vary between
1.5 to 6 liters for an averagely build young patient
20. Once the pressure reaches the pre-set pressure, remove the veress needle and use size 11 blade to
make a smiling skin incision on the infra umbilical crease, to fit a 10mm port. This can be prechecked by placing a 10mm port on the skin for estimation of incision size. Use the tip of an artery
forceps to dilate the urachus as per the Scandinavian technique of primary port placement.
21. Insert the 10mm cannula with trocar by oscillatory screwing motion, the direction being
perpendicular till give way sensation is perceived and then change the direction towards the pelvis.
Once you are in, the trocar should be removed and the telescope should be inserted to confirm the
intraperitoneal placement
22. Connect the insufflator to the optical port and switch on the gas.
23. To begin with, an overview inspection of the entire abdomen must be done and noted.
24. Then reach out to the target organ (fallopian tube of affected side), just about to touch it with the tip
of the telescope, and trans-illuminate the anterior abdominal wall to delineate the site of the target.
25. Use the baseball diamond concept to mark the position of the additional 5 mm ports.
26. The surgeon must use transillumination to avoid any vessel injuries in prospective port sites. Use the
size 11 blade to make small incisions to fit the 5mm ports at the pre-marked sites as per Baseball
diamond concept.
27. Insert both the 5mm ports under direct vision and using principles same as that used for the primary
port to avoid inadvertent visceral and vascular injuries.
Identification of fallopian tube with ectopic pregnancy in situ:
1. find the affected side fallopian tube by using atraumatic grasper and a Maryland as probes only.
The contralateral tube must also be inspected to determine if it is healthy or not.
2. The affected tube is identified and mobilized to minimize bleeding, 5to8 ml diluted solution
containing 5 unit vasopressin in 20 ml of normal saline is injected with a 20 gauge spinal or
laparoscopic needle, Inject vasopressin in the mesosalpinx just below the ectopic and over the
antimesenteric surface of the tubal segment containing the trophoblastic tissue.
3. After stabilizing the tube by grasper in one hand and tritome in other, a linear incision is made on
the antimesenteric surface extending 1-2 cms over the thinnest portion of the tube. follow the
principles of the hook , look and cook while using the energy source.
4. The fine needle tip should be used in the cutting mode, and should barely touch the tissue surface.
5. It is important to remain aware of the location of underlying or adjacent structures..
6. The products of conception usually should protrude through the incision and slowly slip out of the
tube, it may be released gently out using hydro dissection or laparoscopic atraumatic forceps.
7. As pregnancy is pulled out or extruded from the tube it can be placed in a plastic or endobag and
removed through 10mm port on the umbilicus, under vision with the 5mm telescope in the lateral
port.
8. After the pregnancy is removed visualize for hemostasis.
9. The 10mm umbilical port fascia must be closed using a veress needle as a suture passer(Suture
used is vicryl 0.0). remove the optical port slowly with the edge of telescope inspecting the fascial
planes to avoid any bowel herniation.
10. Don’t abruptly remove the primary port
11. Keep the telescope in the abdominal cavity and start withdrawing the cannula
12. Continue to observe this withdrawal process on the monitor
13. Once the cannula has reached within the abdominal wall then start withdrawing the telescope
14. Remove the cannula and the Telescope under vision.
15. This process will avoid entrapment of Omentum or Bowel within the Primary port wound
16. Primary Port fascia and Skin closed; Secondary Port Skin should be closed
17. The skin should be closed with a fine Monofilament suture
18. Abdomen cleaned and Port site wound dressing applied
19. The patient is monitored by the anesthesia team and post-operative vitals are noted.
Tissue retrieved must be sent for histopathological examination. Provide Surgery Photos or Surgical Video to the patient. Provide Discharge Summary documenting Institute findings of the surgery.