Task Analysis Of Laparoscopic Sleeve Gastrectomy
BY DR. SUNILA DAYARAM SEWANIMBBS, MS (GENERAL SURGERY), FIAGES, FMAS, DMAS
PROCEDURAL STEPS:
1. General anesthesia and insertion of Foley’s catheter and nasogastric tube
2. Part preparation and patient positioning
3. Position of surgical team and equipment
4. Creation of pneumoperitoneum and port insertion
5. Retraction of liver
6. Identifying the lower limit of the gastric pouch
7. Dealing with the short gastric arteries along the greater curvature of the stomach
8. Mobilizing the posterior surface of the stomach
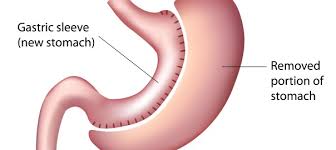
9. Dealing with hiatus hernia, if present
10. Gastric transaction according to the gastric calibration tube
11. Checking for hemostasis and leakage
12. Extraction of the specimen
13. Port closure
14. Post-operative care
EXECUTION STEPS:
1. General anesthesia and insertion of Foley’s catheter and nasogastric tube.
a. The patient is administered general anesthesia depending on the anesthetist’s preference and evaluation of the patient.
b. A nasogastric tube is inserted and its position confirmed by pushing air through it and auscultating a bubbling noise over the right hypochondriac region. It is later fixed securely and gastric decompression is done.
c. An appropriate sized Foley’s catheter is inserted under aseptic precautions and connected to the Urobag. The bulb of Foley’s catheter is inflated with saline after urine can be seen coming out from the catheter. The volume of urine is noted and the bladder is emptied.
2. Port Preparation and patient positioning
a. The area chest, armpits, and the abdomen is prepared intra-operatively by clippers.
b. The patient is initially placed in a supine position with open legs, which will be changed to reverse Trendelenburg (30o head up) after insertion of ports.
c. After painting the operative area with povidone-iodine, the patient is adequately draped, keeping a screen between the head of the patient and the operative field.
d. Pneumatic stockings are tied on the patient’s legs and adequate padding is given to pressure points. DVT prophylaxis is also given.
3. Position of surgical team and equipment
a. The surgeon stands in between the legs of the patient
b. The first assistant can double up as a camera person and he stands to the right of the patient.
c. The 2nd assistant retracts the stomach and stands to the left of the patient.
d. There are 2 monitors placed near each shoulder of the patient.
e. The anesthetist stands towards the head end of the patient along with the anesthetist trolley.
f. The scrub nurse stands near the left leg of the patient along with the instrument trolleys.
4. Creation of pneumoperitoneum and port insertion
a. In the supine position, a stab incision of 2 mm is put 22.5 cms below the xiphoid process in the midline and slightly towards the left side to avoid the fatty and vascular falciform ligament.
b. Veress needle is checked for patency and the spring action.
c. The Veress needle is held like a dart between the pulps of 4 fingers and thumb and is inserted perpendicularly.
d. The unguarded shaft should be (4 cm + abdominal wall thickness), to accommodate the 3-4 cm tenting of the peritoneum.
e. After 2 clicks, the saline aspiration and irrigation test should be performed, followed by a hanging drop test and plunger test, to confirm the intraperitoneal location of Veress’ tip.
f. The CO2 insufflation is started at a flow rate of 1L/min, with the Veress needle held obliquely. The maximum pressure is set to 12mmHg.
g. After the pressure stabilizes, the Veress needle is withdrawn and the incision is lengthened to accommodate a 12 mm optical port. (PORT A)
h. A diagnostic laparoscopy is first performed by visualizing all the quadrants of the abdomen using a 30o or 45o HD laparoscope, inserted through the optical port.
i. The remaining ports are inserted in the following manner according to the Baseball Diamond concept, under vision.
j. The Right Hand Port (12mm) is inserted in the left midclavicular line,
10 cms lateral to the optical port. (PORT B)
k. The Left Hand Port (5mm) is inserted in the right midclavicular line, 10 cms lateral to the optical port. (PORT C)
l. A 5mm port is inserted in the midline near the xiphoid process slightly towards the right side for Nathanson’s liver retractor. (PORT D)
m. A 5mm port is inserted in anterior axillary line 7 cm lateral to the Right Hand Port to retract the stomach. (PORT E)
n. After port insertion, the patient position is changed to 30o reverse Trendelenburg position, to displace the transverse colon and small intestine inferiorly.
5. Retraction of the liver using Nathanson’s liver retractor
a. Nathanson’s liver retractor is inserted from the 5mm subxiphoid port and is used to retract the left lobe of liver from obscuring the view of the left crus of the diaphragm.
6. Identifying the lower limit of the gastric pouch
a. The anterior vein of Mayo overlies the pylorus and is visualized.
b. A sterile tape of 6 cm is inserted and a portion of greater curvature measured carefully starting proximally from the vein of Mayo.
c. Using a monopolar hook or Harmonic ultrasonic scalpel, a window is created in the omental bursa just adjacent to the greater curvature of the stomach at 6 cm mark and the lesser sac is entered.
7. Dealing with the short gastric arteries along the greater curvature of the stomach
a. Using Ligasure, the short gastric arteries are transected close to the greater curvature of the stomach, till the fundus of the stomach has been reached. The assistant should perform traction from the omentum.
b. The spleen and short vessels should be kept in mind. The goal is to expose the cardia and the left crus.
c. The angle of His is opened entirely while dividing the short gastric arteries in the cephalad direction around the fundic area.
8. Mobilization of the posterior surface of the stomach
a. Now the stomach should be retracted towards the patient’s right.
b. The stomach should be individualized from the retroperitoneal organs to achieve correct exposure during the gastrectomy.
c. The spleen and short vessels should be kept in mind. The goal is to expose the cardia and the left crus.
d. The final posterior short gastric can be divided along the left crus.
e. The anterior fat pad is often enlarged and obstructs the view of the medial cardia and the distal esophagus. Mobilize this to provide adequate exposure of this area for optimal stapling and placement of sutures.
9. Dealing with hiatus hernia, if present
a. After opening the angle of His and exposing the left crus, a hiatus hernia will be identified if present.
b. If present, the contents should be reduced into the abdomen and the two crura approximated with interrupted non-absorbable sutures, depending on the size of the hernia. A large hernia may even require a mesh for a tension-free repair of the hernia.
10. Gastric transection according to gastric calibration tube.
a. A 36F gastric calibration tube is inserted by the anesthetist into the stomach and is adjusted along the lesser curvature so as to prevent looping of the tube.
b. An endo-GIA stapler is now introduced via the Right Hand Port.
c. The left-hand grasps the lesser curvature, while the assistant retracts the greater curvature laterally.
d. When adequate care has been taken that there is no vigorous lateral traction on the greater curvature (to prevent the development of functional stenosis in the body of the stomach), the stapler is fired, after confirming that the arms contain only the stomach.
e. The arms of the stapler are kept closed for around 40-60 seconds, so as to ensure hemostasis of the cut margins.
f. Depending on the size of the stomach, multiple stapler firings may be required.
g. After the stapler crosses the first gastric pedicle, the stapler is advanced towards the spleen rather than a gastroesophageal junction, so as to avoid bleeding and leakage from the most-proximal part of the stapler line.
11. Checking for hemostasis and leakage
a. After the new stomach is created, the stapled line should be inspected for bleeding. If there is bleeding, titanium clips or sutures can be applied.
b. Dilute methylene blue is now instilled in the neostomach to watch for any leakage. The maximum capacity of the neostomach is less than 150ml. The stapled line can also be tested for leakage through insufflations with the gastroscope while the remnant stomach is submerged under irrigation fluid.
12. Extraction of the specimen
a. The Right Hand Port is utilized to extract the specimen.
b. The specimen is first introduced inside an endobag.
c. It is then extracted through the Right Hand Port along with the cannula.
d. If there is any difficulty in extracting the specimen, the fascia can be enlarged using a Kelly clamp or medium-sized artery forceps introduced alongside of the cannula.
13. Port closure
a. The insufflation is stopped after the procedure and all instruments are removed from the cannula, to allow the abdomen to decompress homogenously.
b. The ports are then removed under vision.
c. Finally, the optical port is removed and closed with trans fascial Vicryl suture using a knot pusher, followed by subcuticular skin sutures.
d. All the ports 10mm or larger are closed in 2 layers like the optical port. Smaller ports are sutured in a single layer of subcuticular stitches.
e. The sutures are covered with sterile tapes.
14. Post-operative care
a. On POD-1, patients undergo a gastrograffin study to check for any leakage from the staple line.
b. The patient is then started on oral fluids following a normal gastrograffin study.
c. If pain is adequately controlled on oral analgesics, the patient is discharged on POD-3 after explaining dietary and medication advice.
d. Follow-ups are arranged on POD-7 and POD-10.