MBBS, MS
World Laparoscopy Hospital
(December 2016 batch)
REVIEW OF GERD
Gastroesophageal reflux disease (GERD) also known as acid reflux, is a long term condition where stomach contents come back up into the esophagus resulting in either symptoms or complications. Symptoms include the taste of acid in the back of the mouth, heartburn, bad breath, chest pain, vomiting, breathing problems, and wearing away of the teeth. Complications include esophagitis, esophageal strictures, and Barrett's esophagus.
Risk factors include:
- Obesity,
- Pregnancy,
- Smoking,
- Hiatus hernia,and
- Medications (antihistamines, calcium channel blockers, antidepressants,etc )
Goals in surgery:
The standard surgical treatment for severe GERD is the Nissen fundoplication. In this procedure, the upper part of the stomach is wrapped around the lower esophageal sphincter to strengthen the sphincter and prevent acid reflux and to repair a hiatal hernia. It is recommended only for those who are refractory to medical treatment and not to those patients who are resistant to medical therapy.
Final goal after laparoscopic fundoplication are:
1. Symptomatic relief from GERD
2. No dysphagia symptoms postoperatively
3. Reduced intra operative complications
4. Reduced post operative hospital stay
TASK ANALYSIS:
1. Procedural steps
2. Executional steps
Procedural steps:
1. General anaesthesia followed by Patient positioning,
2. Cleaning and sterile draping
3. Co2 Insufflation via veress needle at 5cm superior to umbilicus
4. Insertion of ports
5. Liver retraction by Nathenson’s retractor and identification of pars flacida
6. Exposing the right and left crura of the diaphragm
7. Mobilisation of oesophagus upto 5cm intra-abdominally
8. Approximating the gap between both crura through sutures
9. Mobilisation and preparation of stomach for wrapping by dividing short gastric vessels
10. Plication of fundus of stomach around mobilised oesophagus
11. Inspection of tightness of fundoplication
12. Irrigation and suction
13. Haemostasis achieved
14. Removal of ports under vision
15. Skin closure
Executional steps:
Anesthesia:
General anesthesia
Patient Position:
1. Patient is placed in supine position with legs in lithotomic position.
2. Operating table height must be 0.49 x surgeon height
3. The operation table is tilted approximately 15° head up.
4. The surgeon stands in between patient’s leg.
5. First assistant with telescope and video camera stands on the left of patient.
6. Scrub nurse along with instrument trolley stands on the left of patient next to first assistant.
7. Video monitor is positioned at the head end on either side of patient shoulder.
8. The monitor should be placed at a distance of 5 times multiplied by the diagonal measurement of monitor screen and should be at a height of approximately 10° lower from the surgeons eye
9. The surgeon, target organ (gastro oesophageal junction), and monitor are to be present in a co-axial alignment.
Port position:
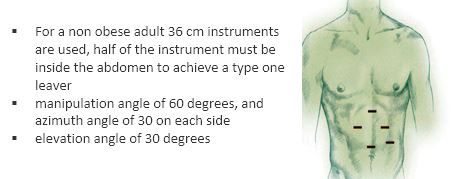
1. All ports are made according to “ base ball diamond concept”
2. 10 mm optical port should be placed 5 cm above the umbilicus
3. 5 mm port on right hypochondria 7.5 cm away from optical port
4. Another 5mm port is made on left hypochondria 7.5 cm away from optical port.
5. One more 5mm port is made in left mid-clavicle line just below the left costal margin.
6. A 5th port of 5mm calibre for Nathensson’s retractor is made in epigastric region.
Quadro manometric settings are assessed.
1) Pre set pressure is maintained at 15 mm of Hg.
2) Cautery check with monopolar and patient return plate , harmonic device connections are confirmed.
3) Light source and coaxial alignment with surgeon are checked.
4) Co2 cylinder checked for availability of sufficient Co2 for insufflation.
5) Working status of all the lap instruments along with insulation check is properly made.
Operative steps:
Access and Insufflation
1. Check veress needle for patency and spring action
2. A small stab incision using number 11 blade at 5cm superiorly to the umbilicus is made
3. Lift the lower abdominal wall between your palm and four fingers
4. Measure the thickness of the abdominal wall
5. Hold the veress needle like a dart exposing only 4cm + the measured abdominal wall thickness, and direct it at 45 degrees to the patient abdominal axis yet 90 degrees to the abdominal wall aiming towards the anus
6. You must feel two give away clicks
7. Make sure you are inside the abdominal cavity using the following tests :
i) Irrigation and suction test : free flow of 5cc saline with no resistance, then on suction, only air must come back
ii) Hanging drop test : put one drop of saline at the opening of the veress needle then lift the abdominal wall, the drop must go through the needle
iii) Connect to the insufflator : intra-abdominal pressure must be zero
8. Start insufflation with Co2 gas at flow rate of 1L/min and keep an eye on the quadromanometric readings on the insufflator to make sure that the rise in the intra abdominal pressure is proportional to the total amount of gas pumped
i) When reaching 12 mmHg pressure enlarge your incision to 1.1 cm, then insert a size 10mm port at 90 degrees using screw movement to the right and left
9. Remove the trocar and connect the gas tube to the port
10. Connect the 30° telescope to camera head and make sure that white balance setting is achieved
11. Insert the telescope into the abdominal cavity above the umbilicus, inspect all four quadrants and the abdominal cavity for any other pathology
Liver retraction: Through the epigastric 5mm port a Nathensson’s self retaining retractor is introduced and liver is lifted and retracted exposing the gastro-esophageal junction and pars flacida ligament
Dissection:
Identification of Pars flacida:
After liver is retracted using Nathensen’s self retaining retractor, pars flacida is identified as it is the most thin layer of peritoneum devoid of any fat,
Dissection is started by dividing this layer and exposing the caudate lobe of the liver.
Just medial to caudate lobe lies the inferior vena cava, so care should be taken not to dissect in this area and to avoid overshooting of the instruments.
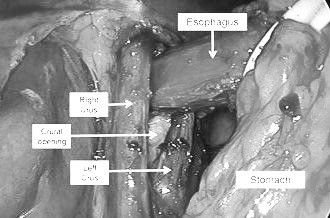
Identification and dissection of both right and left crus of diaphragm:
Stomach is retracted antero laterally using an atraumatic grasper by the assistant so that right crus of diaphragm is exposed.
Dissection is carried on carefully to delineate the right crus, using diathermy/ harmonic scalpel and dissecting forceps.
The loose areolar tissue between the right crus and the esophagus is dissected carefully, taking note of not injuring the posterior vagal trunk and avoiding perforation of the esophagus.
After dissecting right crus, stomach is retracted antero medially to expose the left crus of diaphragm. Careful dissection using diathermy/harmonic and scissors will delineate the left crus.
Mobilization of esophagus:
Anterior mobilization of the oesophagus is done and care must be taken to avoid undue cutting of anterior vagus which runs on the anterior wall of the oesophagus, slightly embedded in it.
Posterior mobilization of the oesophagus is done to form a window for stomach to insert a sling and the posterior vagus nerve is visualized which lies just on the posterior wall of oesophagus.
Insertion of a sling:
A sling is passed through a separate punctured wound from abdominal wall without inserting a separate port.
A grasping forceps is inserted through one of the port to hold the sling so that the oesophagus can be manipulated.
The gastro-esophageal junction is retracted by the help of the sling in antero medial pull.
The surroundings of oesophagus in the posterior mediastinum is dissected for 5- 6 cm.
Mobilization of stomach:
The fundus part of the stomach is mobilized nicely along with the gastro esophageal junction by antero medial traction
Sling for retraction of esophagus is released at this point of time
The short gastric vessels are separated with the help of a bipolar or harmonic scalpel which aids in further mobilization of the fundus of the stomach through the earlier formed posterior window.
Care must be taken not to injure the spleen which is adjacent to the stomach.
A grasper is advanced through the posterior window and the Posterior wall of the fundus is held and pulled through the window from right side to the left.
Perform a Shoe shine maneuver to form a FLOPPY NISSEN.
Floppy Nissen has less chances of dysphagia which is the effect of tight wrap of the fundus.
After doing a floppy wrap of fundus around the mobilized esophagus a buttock sign with posterior wall of the fundus is ascertained to confirm the adequacy of the wrap
Crural approximation:
With the lower end of mobilized esophagus, g- junction and the fundus of the stomach retracted antero laterally, both the crura are identified and approximated for suturing.
The right and left crura are approximated with two or three surgeons knots or Tumble Square Knot with Ethibond which is a non absorbable suture.
Care must be taken not to tightly approximate the crura and atleast 5 mm gap must be left between the oesophagus and the knots to avoid dysphagia.
Fundoplication:
Sling for retraction of esophagus is released at this point of time
By using a atraumatic grasper in the left hand, the posterior wall of the fundus is held through the opening made behind the esophagus.
The posterior wall of fundus is pulled gently and at the same time the extra anterior wall is pushed back to avoid crowding of tissue with in the window.
By serial movements of pulling posterior wall forward and pushing anterior wall back, a sufficient amount of wrap is made around the esophagus, this can be ascertained by seeing the ‘buttock sign’.
The wrap made by both posterior and and anterior wall of fundus shoud not be too tight,
A Floppy Nissen’s is made by doing the ‘shoe shine’ maneuver.
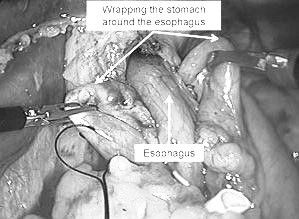
Fixation of wrap by intra-corporeal sutures:
Suture material used is non absorbable suture- Dacron, silk, polypropylene, etc
Approximately 5cm of mobilized esophagus should be prepared for fundal wrap.
First suture is taken with full thickness of anterior wall of fundus and full thickness of posterior wall of fundus is taken
Intra corporeal surgeons knot are used for placating the stomach on to the esophagus, though ‘tumble square knots’ can also be used.
Two suture are taken above the first knot at a distance of 1cm between each knot, involving full thickness of anterior wall of fundus, partial muscular layer of esophagus and full thickness posterior wall of fundus .
In the above suture wall of esophagus is sandwiched between walls of fundus,
Taking full thickness of esophagus in above sutures should be avoided as it may cause a complication of perforation of esophagus
Two sutures are taken below the first knot at a distance of 1cm between each knot in similar manner.
Completing the surgery:
The needle used for suturing is taken out
The the operated area is slightly irrigated and suctioned to clean the area from any oozed blood and clots, and to check for any fresh oozing,
Hemostasis is achieved
Nathensen’s retractor is taken off and liver is brought down in its anatomical position
All the cannula are withdrawn under vision, pneumo peritoneum is undone completely and both the 10 mm port site are closed using vicryl no 1 with the help of suture passer instrument.
Closure of 10 mm ports is to be done under telescopic vision to avoid inadvertent injury to intra abdominal structures.
Skin closure done with skin stapler/ethilon suture no 3-0 in mattress type suture.
Apply adhesive sterile dressing over the wound.
Complications:
Complications of laparoscopic surgery are mainly divided into three groups:
Complications derived from pneumoperitoneum,
Complications caused by the operative procedure and
Postoperative complications.
Apart from the alterations caused by the pneumoperitoneum (raised intraabdominal pressure and physiological effects especially within cardiovascular and respiratory systems), which have significant effects on the patient, especially if they are elderly or have associated morbidity, it may cause some complications such as
Severe hypercarbia,
Cardio-pulmonary compromise,
Air embolism or gas migration (subcutaneous emphysema, pneumo-mediastinum and pneumothorax.
Complications of access or trocar entry include:
Hollow or solid viscus perforation, abdominal wall or major vessel injury, incisional hernia
Complications derived from the surgical technique include:
Hemorrhage, vascular injury, retroperitoneal hematoma.
Nissen (floppy) fundoplication is generally considered to be safe and effective, with a mortality rate of less than 1%.
Studies have shown that after 10 years, 89.5% of patients are still symptom-free.
Complications include gas bloat syndrome", dysphagia, dumping syndrome, excessive scarring, vagus nerve injury, and rarely, achalasia.
. So thanks For Dr Pawan Kumar Hosamani