DR. MOHAMMAD FAROOQUE
DEPARTMENT OF GENERAL SURGERY
SUMANDEEP VIDYAPEETH
GUJARAT
1. After successful pneumoperitoneum with veress, an 11mm smiling incision is made in the inferior crease of the umbilicus using no.11scalpel.
2. Use mosquito forceps to dilate the obliterated Vitello intestinal duct (Scandinavian technique).
3. Insert the 10 mm cannula with trocar with guarded screwing movement, perpendicular to the abdominal wall till give away sensation is perceived.
4. Remove the trocar and push the cannula in.
5. Introduce the 30-degree telescope in after white balancing and focussing at 10 cm distance and visualise the area directly under the port for presence of any bleeding or injury.
6. Transilluminate the abdominal wall and insert one 10 mm port on the left and one 5mm port on the right under vision by the Baseball Diamond concept. You can also use the ipsilateral port with a 7.5 cm distance in between.
7. Do a complete examination of the abdomen and pelvis and push the bowel above the sacral promontory.
8. If the patient has a uterus that is affecting exposure, it can be retracted with a stitch to the anterior abdominal wall.
9. Dissection is started posteriorly(Holy plane of Heald). The plane between the mesorectum and retroperitoneum is identified; the retroperitoneum is usually whiter than the mesorectum.
10. A harmonic scalpel is used to enter the posterior pelvic plane under the superior rectal artery, and the left ureter and hypogastric nerve plexus are identified.
11. Dissection is extended downward through the presacral anatomic space, all the way to the pelvic floor.
12. The dissection must be carried below the rectosacral (Waldeyer) fascia. Often, to facilitate exposure, the right lateral stalk of the rectum is also mobilized.
13. Once the right stalk and posterior areas are mobilized, dissection proceeds anteriorly into the rectovaginal plane.
14. Subsequently, the rectum is mobilized anteriorly to the upper limit of the vagina. During this approach, the nervi erigentes and left lateral ligament are spared.
15. The rectum is then pulled out of the pelvis, and where the fixation will occur is assessed.
16. A window is made on the left side of the rectum to facilitate the rectopexy and dissection on sacral promontory is done to expose it.
17. Posterior placement of mesh approximately of size 12*8 cm is done inserted via the right-lower-quadrant port and is placed all the way down to the pelvic floor, extending cephalad behind the mesorectum.
18. The mesh should cover the posterior part of rectum and some of the lateral stalks of rectum.
19. An overly tight pexy must be avoided to prevent obstruction of the rectosigmoid junction. If suturing is chosen, then use Ethibond suture.
20. It is important to identify the sacral venous plexus before tacking or suturing. The bony promontory and presacral fascia is the ideal location for fixation.
21. Then the mesh is fixed on right and left lateral stalks of rectum with the sutures.
22. Close the fold of peritoneum by continuous intracorporeal suturing so that the mesh is extraperitonealised. You can also use Dundee jamming knot with Aberdeen termination. Care should be taken not to include the mesh while suturing the peritoneum.
23. Desufflation of abdomen done
24. Ports are withdrawn under direct visualisation and optical cannula is withdrawn by sliding over the telescope.
25. Skin incisions are either sutured or stapled.
26. Abdomen is cleaned.
27. Antiseptic dressing done
28. Post-op vitals are noted and the patient is shifted to the recovery room.
Elaborated Steps
Position the patient in the lithotomy position.
Administer general anesthesia.
Secure the endotracheal tube.
Place a Foley catheter.
Preoperative antibiotics are administered.
The abdomen is insufflated using CO2.
The laparoscope is inserted through a 10mm port at the umbilicus.
Place 3-4 additional trocars as required.
The small intestine is retracted to expose the retrorectal area.
The rectum is mobilized by incising the peritoneal reflection.
Mobilize the sigmoid colon by dividing the white line of Toldt.
Identify the sacral promontory.
Dissect behind the rectum to create a tunnel that extends from the sacral promontory to the levator ani muscles.
Insert the mesh into the tunnel created behind the rectum.
Anchor the mesh to the sacral promontory using non-absorbable sutures.
Anchor the mesh to the levator ani muscles using non-absorbable sutures.
Check the position of the mesh to ensure that it is correctly placed and not twisted.
Retract the mesh to ensure that it is taut and not loose.
Inspect the mesh for any defects or tears.
Remove the laparoscope.
Close the ports.
Deflate the abdomen.
Remove the trocars.
Close the incisions with sutures or staples.
Apply sterile dressing to the incisions.
The patient is awakened from anesthesia.
Extubate the endotracheal tube.
Move the patient to the post-anesthesia care unit.
Administer analgesics for pain management.
Monitor vital signs and urine output.
Check the dressing for bleeding or drainage.
Observe the patient for any signs of infection or complications.
Initiate a clear liquid diet.
Remove the Foley catheter once the patient is able to void.
Discharge the patient when stable.
Instruct the patient on postoperative care.
Prescribe antibiotics and analgesics as needed.
Instruct the patient to avoid strenuous activity for 2-4 weeks.
Advise the patient to eat a high-fiber diet and drink plenty of fluids.
Advise the patient to avoid constipation and straining during bowel movements.
Schedule a follow-up appointment.
Evaluate the patient's postoperative course.
Monitor for any complications, such as bleeding or infection.
Evaluate the patient's bowel function.
Adjust medication as needed.
Evaluate the healing of the incisions.
Monitor the patient for any signs of mesh erosion or bowel obstruction.
Recommend physical therapy as needed.
Provide the patient with a detailed report of the procedure and postoperative care.
Advise the patient on any potential complications or side effects of the procedure.
Provide the patient with instructions on follow-up appointments and monitoring.
Advise the patient on when to resume normal activities, such as driving, work, and exercise.
The patient follows up with the surgeon at regular intervals.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment and provides any further treatment as necessary.
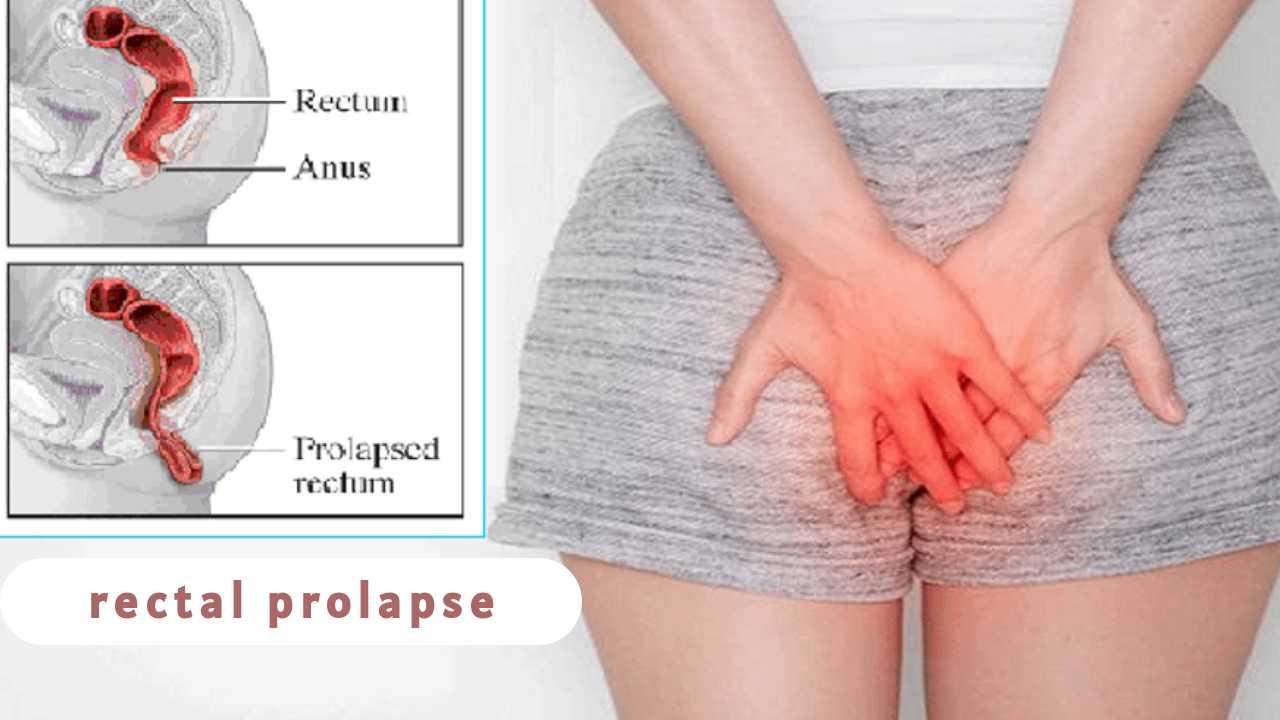
Rectal prolapse is a debilitating condition that affects 1% of people older than 60 years. Surgical approaches to its treatment include a perineal approach and an abdominal approach. Laparoscopic rectopexy was initially described in the early 1990s and has since become the abdominal procedure of choice for rectal prolapse.
Indications:
Once rectal prolapse is diagnosed, surgical repair is indicated to prevent worsening fecal incontinence and discomfort.
BEAHRS ET AL CLASSIFICATION:
1. Incomplete (Mucosal Prolapse)
2. Complete (Full thickness wall prolapsed)
First degree: High or Early, “Concealed”, “Invisible”
Second degree: Externally visible on straining, sulcus evident between rectal wall and anal canal
Third degree: Externally visible
Patient Preparation:
- Proper history taking and clinical examination of the patient
- Routine investigations and additional investigations based on comorbidities
- Anesthetic fitness
- Informed Consent
In preparation for the procedure, the patient is kept on NPO (nil per os) status, beginning the night before surgery. Prophylactic antibiotics are given per Surgical Care Improvement Project (SCIP) criteria.
Periprocedure:
A Foleys catheter is inserted for the duration of the case but is removed before extubation. Clippers are used to remove abdominal wall hair.
Patient Position:
The patient is placed in modified Lloyd Davis position(head down lithotomy) to make bowel fall away from the operative site. Special attention is given to the legs, avoiding excessive posterior or lateral compression, sparing any injuries to the calf muscle and lateral superficial peroneal nerve.
STEPS:
2. Use mosquito forceps to dilate the obliterated Vitello intestinal duct (Scandinavian technique).
3. Insert the 10 mm cannula with trocar with guarded screwing movement, perpendicular to the abdominal wall till give away sensation is perceived.
4. Remove the trocar and push the cannula in.
5. Introduce the 30-degree telescope in after white balancing and focussing at 10 cm distance and visualise the area directly under the port for presence of any bleeding or injury.
6. Transilluminate the abdominal wall and insert one 10 mm port on the left and one 5mm port on the right under vision by the Baseball Diamond concept. You can also use the ipsilateral port with a 7.5 cm distance in between.
7. Do a complete examination of the abdomen and pelvis and push the bowel above the sacral promontory.
8. If the patient has a uterus that is affecting exposure, it can be retracted with a stitch to the anterior abdominal wall.
9. Dissection is started posteriorly(Holy plane of Heald). The plane between the mesorectum and retroperitoneum is identified; the retroperitoneum is usually whiter than the mesorectum.
10. A harmonic scalpel is used to enter the posterior pelvic plane under the superior rectal artery, and the left ureter and hypogastric nerve plexus are identified.
11. Dissection is extended downward through the presacral anatomic space, all the way to the pelvic floor.
12. The dissection must be carried below the rectosacral (Waldeyer) fascia. Often, to facilitate exposure, the right lateral stalk of the rectum is also mobilized.
13. Once the right stalk and posterior areas are mobilized, dissection proceeds anteriorly into the rectovaginal plane.
14. Subsequently, the rectum is mobilized anteriorly to the upper limit of the vagina. During this approach, the nervi erigentes and left lateral ligament are spared.
15. The rectum is then pulled out of the pelvis, and where the fixation will occur is assessed.
16. A window is made on the left side of the rectum to facilitate the rectopexy and dissection on sacral promontory is done to expose it.
17. Posterior placement of mesh approximately of size 12*8 cm is done inserted via the right-lower-quadrant port and is placed all the way down to the pelvic floor, extending cephalad behind the mesorectum.
18. The mesh should cover the posterior part of rectum and some of the lateral stalks of rectum.
19. An overly tight pexy must be avoided to prevent obstruction of the rectosigmoid junction. If suturing is chosen, then use Ethibond suture.
20. It is important to identify the sacral venous plexus before tacking or suturing. The bony promontory and presacral fascia is the ideal location for fixation.
21. Then the mesh is fixed on right and left lateral stalks of rectum with the sutures.
22. Close the fold of peritoneum by continuous intracorporeal suturing so that the mesh is extraperitonealised. You can also use Dundee jamming knot with Aberdeen termination. Care should be taken not to include the mesh while suturing the peritoneum.
23. Desufflation of abdomen done
24. Ports are withdrawn under direct visualisation and optical cannula is withdrawn by sliding over the telescope.
25. Skin incisions are either sutured or stapled.
26. Abdomen is cleaned.
27. Antiseptic dressing done
28. Post-op vitals are noted and the patient is shifted to the recovery room.
Elaborated Steps
Position the patient in the lithotomy position.
Administer general anesthesia.
Secure the endotracheal tube.
Place a Foley catheter.
Preoperative antibiotics are administered.
The abdomen is insufflated using CO2.
The laparoscope is inserted through a 10mm port at the umbilicus.
Place 3-4 additional trocars as required.
The small intestine is retracted to expose the retrorectal area.
The rectum is mobilized by incising the peritoneal reflection.
Mobilize the sigmoid colon by dividing the white line of Toldt.
Identify the sacral promontory.
Dissect behind the rectum to create a tunnel that extends from the sacral promontory to the levator ani muscles.
Insert the mesh into the tunnel created behind the rectum.
Anchor the mesh to the sacral promontory using non-absorbable sutures.
Anchor the mesh to the levator ani muscles using non-absorbable sutures.
Check the position of the mesh to ensure that it is correctly placed and not twisted.
Retract the mesh to ensure that it is taut and not loose.
Inspect the mesh for any defects or tears.
Remove the laparoscope.
Close the ports.
Deflate the abdomen.
Remove the trocars.
Close the incisions with sutures or staples.
Apply sterile dressing to the incisions.
The patient is awakened from anesthesia.
Extubate the endotracheal tube.
Move the patient to the post-anesthesia care unit.
Administer analgesics for pain management.
Monitor vital signs and urine output.
Check the dressing for bleeding or drainage.
Observe the patient for any signs of infection or complications.
Initiate a clear liquid diet.
Remove the Foley catheter once the patient is able to void.
Discharge the patient when stable.
Instruct the patient on postoperative care.
Prescribe antibiotics and analgesics as needed.
Instruct the patient to avoid strenuous activity for 2-4 weeks.
Advise the patient to eat a high-fiber diet and drink plenty of fluids.
Advise the patient to avoid constipation and straining during bowel movements.
Schedule a follow-up appointment.
Evaluate the patient's postoperative course.
Monitor for any complications, such as bleeding or infection.
Evaluate the patient's bowel function.
Adjust medication as needed.
Evaluate the healing of the incisions.
Monitor the patient for any signs of mesh erosion or bowel obstruction.
Recommend physical therapy as needed.
Provide the patient with a detailed report of the procedure and postoperative care.
Advise the patient on any potential complications or side effects of the procedure.
Provide the patient with instructions on follow-up appointments and monitoring.
Advise the patient on when to resume normal activities, such as driving, work, and exercise.
The patient follows up with the surgeon at regular intervals.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment and provides any further treatment as necessary.